Difference between revisions of "Journal:Codesign of the Population Health Information Management System to measure reach and practice change of childhood obesity programs"
Shawndouglas (talk | contribs) (Saving and adding more.) |
Shawndouglas (talk | contribs) (Saving and adding more.) |
||
| Line 145: | Line 145: | ||
|} | |} | ||
|} | |} | ||
===Technical requirements and specifications=== | |||
The business analysis stage of the project identified two key requirements of the system: to support local delivery of HCI programs across NSW by providing contact management and scheduling capabilities for health promotion officers (HPOs); and to support the Ministry performance management framework.8 | |||
The system uses a Windows-based application that uses Microsoft Dynamics Customer Relationship Management (CRM), Select Survey (questionnaire component), SSRS (SQL Server Reporting Services) for reporting, and a state-wide login service. | |||
===User acceptance testing=== | |||
User input and feedback was obtained from state-level program managers and through demonstration visits with LHD health promotion services. This ensured user needs were met and questions about the new system were addressed. | |||
===Training and deployment=== | |||
Deployment of PHIMS was supported by representatives from each of the 15 LHDs (referred to as "champions") and 11 staff within the Ministry. The business analyst conducted a two-day training course with the LHD champions and Ministry staff. Then, prior to system deployment, webinar training was conducted for each LHD, consisting of 40 sessions (lasting one to two hours each) with approximately 100 attendees. A set of tip sheets was also developed. | |||
The system was deployed in six stages from August 2014, starting with a pilot in one LHD and subsequent sequential roll-out to the remaining 14 LHDs, completed in September 2014. | |||
Data cleaning and migration took more than 12 months, running in parallel with the build, user acceptance testing, and deployment stages. Identifying and addressing data migration issues was a key factor in the successful deployment of PHIMS. Various interim data systems were in place in LHDs and needed to be integrated during the data migration process. Most issues were noncritical and occurred after data migration or within the first three months after deployment. Most of the system issues (550/566, 97%) had been resolved within 12 months of deployment. | |||
===User interface and reporting=== | |||
The user views a dashboard screen that contains a bulletin board for system announcements, website links, and real-time program adoption graphs for the ''Munch & Move'' and ''LLW@S'' programs. The system is made up of a hierarchy of forms (windows) that present information and enable the user to perform various actions. | |||
PHIMS has the following key features that are used by HPOs to support local implementation of HCI programs: | |||
1. '''Contact management''': supports HPO workflows for managing interactions with sites (i.e., early childhood services and primary schools) and allows the user to record details in the one location. This has improved record keeping and retrieval and is a well-used function of the system with more than 54,000 entries. | |||
2. '''Capacity to record each site’s training''': demonstrates program reach (i.e., sites formally trained in ''Munch & Move'' or ''LLW@S'') | |||
3. '''Scheduled follow-up alerts and recording of program adoption''': alerts an HPO to when a site visit is due at one-, six- and 12-month intervals. During the visit, the HPO collects data on the program practices and enters it into the scheduled follow-up summary form (which links to the questionnaire [Select Survey] component). This data is then used for the performance monitoring reports. Other details from the visits are captured in the contact notes. | |||
4. '''Operational reporting''': allows HPOs to see which sites need additional support. Examples of reports are summaries of training entries, scheduled follow-ups, practice achievement, and program adoption over time. | |||
PHIMS has the capability to support reporting at state level by monitoring program reach (e.g., number of sites trained), practice achievement, and program adoption. | |||
The reports are generated in real time and allow the user to search and display data by specific criteria, for example, NSW, LHD, or local government area, or sites in disadvantaged areas. | |||
==Use of PHIMS== | |||
==Acknowledgements== | ==Acknowledgements== | ||
Revision as of 20:44, 7 January 2019
| Full article title | Codesign of the Population Health Information Management System to measure reach and practice change of childhood obesity programs |
|---|---|
| Journal | Public Health Research & Practice |
| Author(s) |
Green, Amanda M.; Innes-Hughes, Christine; Rissel, Chris; Mitchell, Jo; Milat, Andrew J.; Williams, Mandy; Persson, Lina; Thackway, Sarah; Lewis, Nicola; Wiggers, John |
| Author affiliation(s) |
NSW Ministry of Health, University of Sydney, South Western Sydney Local Health District, Hunter New England Local Health District, University of Newcastle |
| Primary contact | Email: Amanda dot Green at health dot nsw dot gov dot au |
| Year published | 2018 |
| Volume and issue | 28(3) |
| Page(s) | e2831822 |
| DOI | 10.17061/phrp2831822 |
| ISSN | 2204-2091 |
| Distribution license | Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International |
| Website | http://www.phrp.com.au/issues/september-2018-volume-28-issue-3/ |
| Download | http://www.phrp.com.au/wp-content/uploads/2018/09/PHRP2831822.pdf (PDF) |
|
|
This article should not be considered complete until this message box has been removed. This is a work in progress. |
Abstract
Introduction: Childhood obesity prevalence is an issue of international public health concern, and governments have a significant role to play in its reduction. The Healthy Children Initiative (HCI) has been delivered in New South Wales (NSW), Australia, since 2011 to support implementation of childhood obesity prevention programs at scale. Consequently, a system to support local implementation and data collection, analysis, and reporting at local and state levels was necessary. The Population Health Information Management System (PHIMS) was developed to meet this need.
Design and development: A collaborative and iterative process was applied to the design and development of the system. The process comprised identifying technical requirements, building system infrastructure, delivering training, deploying the system, and implementing quality measures.
Use of PHIMS: Implementation of PHIMS resulted in rapid data retrieval and reporting against agreed performance measures for the HCI. The system has 150 users who account for the monitoring and reporting of more than 6000 HCI intervention sites (early childhood services and primary schools).
Lessons learned: Developing and implementing PHIMS presented a number of complexities including: applying an information technology (IT) development methodology to a traditional health promotion setting; data access and confidentiality issues; and managing system development and deployment to intended timelines and budget. PHIMS was successfully codesigned as a flexible, scalable, and sustainable IT solution that supports state-wide HCI program implementation, monitoring, and reporting.
Introduction
Childhood overweight and obesity is of international public health concern, and governments have a significant role to play in addressing the issue.[1] In New South Wales (NSW), Australia, the prevalence of childhood overweight and obesity remains high, at 21 percent.[2]
From 2011 to 2014, the Australian Government implemented the National Partnership Agreement on Preventive Health, which provided a historic increase in funding to prevent chronic disease. In NSW, this coordinated prevention effort for children was delivered through the Healthy Children Initiative (HCI) by the NSW Ministry of Health (the Ministry). The HCI involves the implementation of primary and secondary obesity prevention programs across the state in settings attended by children, for example, early childhood services and primary schools.[3]
A well-established health promotion workforce existed in NSW that had designed and implemented programs in these settings and had the potential to achieve state-wide population-level reach and outcomes. However, a significant scaling up of delivery and monitoring of these programs was required to effect population-level change. To facilitate this, enhanced funding was provided to all 15 NSW Government Local Health District (LHD) health promotion services to support local implementation of these programs.[4]
Two programs—Munch & Move and Live Life Well @ School (LLW@S)—were identified from pilot programs to be delivered at scale across NSW as part of the HCI. Munch & Move had a potential reach of more than 3,500 center-based early childhood services and more than 190,000 children aged 0–5 years. LLW@S had a potential reach of more than 2,400 primary schools with more than 675,000 students.
Initial implementation of both Munch & Move and LLW@S involved training of educators and teachers to embed the promotion of healthy behaviors in their organizational policy and routine practice. To ensure the successful translation into routine practice, educators and teachers were supported by their local LHD through regular visits or phone calls, and they were monitored through a set of program adoption indicators referred to as "practices." These evidence based practices refer to organizational policies and practices related to nutrition, physical activity, and sedentary behavior (see Tables 1 and 2).[5][6]
| |||||||||||||||||||||
| |||||||||||||||
Consistent with World Health Organization recommendations, a comprehensive HCI monitoring framework was developed to guide the review of program implementation in early childhood services and primary schools. This framework included HCI measures in the annual service agreements between the Ministry (the funder) and LHDs (the providers). Achievement against the measure was reviewed quarterly.
Contemporary and effective delivery of population-level health interventions requires innovative technology and fresh approaches to monitoring and reporting. Conte et al.[7] described the lack of evidence about whether an e-monitoring system improved the implementation of evidence-based preventive programs. However, because performance measures were included in the LHD service agreements, a system was needed to support the implementation of the HCI at the local level, and the collection, recording, analysis, and reporting of this data at both local and state levels. To achieve this, an information technology (IT) system called the Population Health Information Management System (PHIMS) was developed to perform these functions for both LHD and Ministry staff.
Design and development
Governance
In July 2011, a project board was formed with representatives from each of the project stakeholder groups across the Ministry and LHDs. The purpose of the board was to facilitate collaboration and guide the development of an overarching performance monitoring framework. A dedicated business analyst was engaged to consult with future users and to develop the business requirements document.
Development process
Codesign was undertaken between the Ministry and LHDs, who contributed to the development of the business requirements and monitored the implementation of the new system. A third-party vendor was contracted to undertake the build, user acceptance testing, and deployment support.
Development involved an iterative process. The system’s dual purposes (local and state-level application) were first clarified, with subsequent identification of related needs and operational priorities to be included in the business requirements document. This was completed in May 2012 and used by the solution architect and system developers to guide the design of the functional architecture. A commercial off-the-shelf solution was adapted to build a "fit-for-purpose" system that met the needs of stakeholders and could be integrated into an existing organizational system.
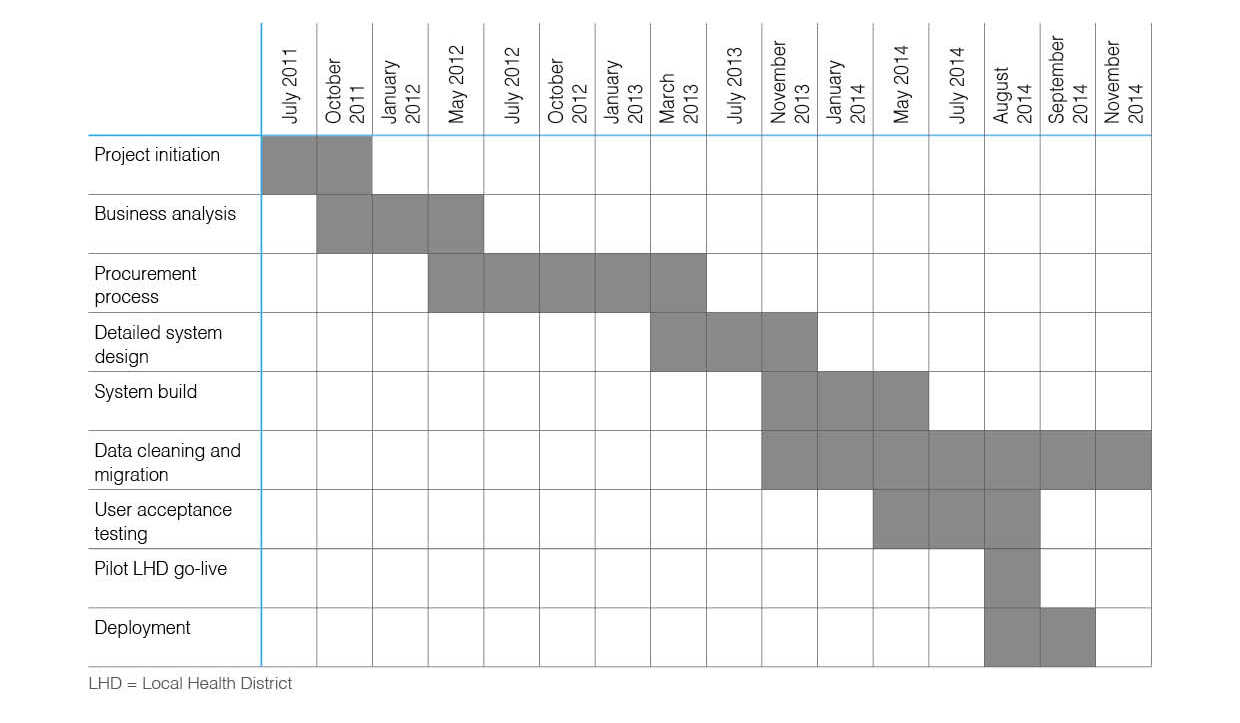
User acceptance testing, training of LHD staff, and deployment followed, with the system going live in August 2014. Project initiation to deployment took just over three years; the stages of development are depicted in Figure 1.
|
Technical requirements and specifications
The business analysis stage of the project identified two key requirements of the system: to support local delivery of HCI programs across NSW by providing contact management and scheduling capabilities for health promotion officers (HPOs); and to support the Ministry performance management framework.8
The system uses a Windows-based application that uses Microsoft Dynamics Customer Relationship Management (CRM), Select Survey (questionnaire component), SSRS (SQL Server Reporting Services) for reporting, and a state-wide login service.
User acceptance testing
User input and feedback was obtained from state-level program managers and through demonstration visits with LHD health promotion services. This ensured user needs were met and questions about the new system were addressed.
Training and deployment
Deployment of PHIMS was supported by representatives from each of the 15 LHDs (referred to as "champions") and 11 staff within the Ministry. The business analyst conducted a two-day training course with the LHD champions and Ministry staff. Then, prior to system deployment, webinar training was conducted for each LHD, consisting of 40 sessions (lasting one to two hours each) with approximately 100 attendees. A set of tip sheets was also developed.
The system was deployed in six stages from August 2014, starting with a pilot in one LHD and subsequent sequential roll-out to the remaining 14 LHDs, completed in September 2014.
Data cleaning and migration took more than 12 months, running in parallel with the build, user acceptance testing, and deployment stages. Identifying and addressing data migration issues was a key factor in the successful deployment of PHIMS. Various interim data systems were in place in LHDs and needed to be integrated during the data migration process. Most issues were noncritical and occurred after data migration or within the first three months after deployment. Most of the system issues (550/566, 97%) had been resolved within 12 months of deployment.
User interface and reporting
The user views a dashboard screen that contains a bulletin board for system announcements, website links, and real-time program adoption graphs for the Munch & Move and LLW@S programs. The system is made up of a hierarchy of forms (windows) that present information and enable the user to perform various actions.
PHIMS has the following key features that are used by HPOs to support local implementation of HCI programs:
1. Contact management: supports HPO workflows for managing interactions with sites (i.e., early childhood services and primary schools) and allows the user to record details in the one location. This has improved record keeping and retrieval and is a well-used function of the system with more than 54,000 entries.
2. Capacity to record each site’s training: demonstrates program reach (i.e., sites formally trained in Munch & Move or LLW@S)
3. Scheduled follow-up alerts and recording of program adoption: alerts an HPO to when a site visit is due at one-, six- and 12-month intervals. During the visit, the HPO collects data on the program practices and enters it into the scheduled follow-up summary form (which links to the questionnaire [Select Survey] component). This data is then used for the performance monitoring reports. Other details from the visits are captured in the contact notes.
4. Operational reporting: allows HPOs to see which sites need additional support. Examples of reports are summaries of training entries, scheduled follow-ups, practice achievement, and program adoption over time.
PHIMS has the capability to support reporting at state level by monitoring program reach (e.g., number of sites trained), practice achievement, and program adoption.
The reports are generated in real time and allow the user to search and display data by specific criteria, for example, NSW, LHD, or local government area, or sites in disadvantaged areas.
Use of PHIMS
Acknowledgements
We acknowledge the contributions of Liz King, Neil Orr, Louise Farrell, Bev Lloyd, Andy Bravo, Masela Draper, Deni Fukunishi, Andy Lui, Rita Lagaluga, Evan Freeman, Elena Ouspenskaia, Claudine Lyons, Kym Buffett, Rhonda Matthews, Project Advisory Board Members, Steering Committee Members, Transition Group and Reference Group Members and the Directors and staff of Local Health District Health Promotion Services across NSW.
This paper was developed as part of a program of research on monitoring health promotion practice within The Australian Prevention Partnership Centre. It was funded through the National Health and Medical Research Council Partnership Centre Grants Scheme (ID GNT 9100001) with the Australian Government Department of Health, the NSW Ministry of Health, ACT Health and the HCF Research Foundation.
Author contributions
AG and CI-H drafted the manuscript. CR, JM, AM, MW, LP, ST, NL and JW reviewed and contributed to editing the manuscript. All authors read, revised and approved the final manuscript. All authors contributed to the development and/or implementation of PHIMS.
Competing interests
None declared.
Peer review and provenance
Externally peer reviewed, commissioned.
References
- ↑ Commission on Ending Childhood Obesity (2016). Report on the Commission on Ending Childhood Obesity. World Health Organization. pp. 50. ISBN 9789241510066. http://apps.who.int/iris/bitstream/handle/10665/204176/9789241510066_eng.pdf;jsessionid=4EA7FECA778E7E3B8C7BA4420E1B2412?sequence=1. Retrieved 07 February 2018.
- ↑ "Overweight and obesity in children aged 5–16 years, NSW 2007 to 2017". HealthStats NSW. NSW Government. 8 May 2018. http://www.healthstats.nsw.gov.au/Indicator/beh_bmikid_cat. Retrieved 10 July 2018.
- ↑ Innes-Hughes, C.; Bravo, A. Buffett, K. et al. (2017). NSW Healthy Children Initiative: The first five years July 2011 – June 2016. NSW Ministry of Health. pp. 43. ISBN 9781760007263. https://www.health.nsw.gov.au/heal/Publications/HCI-report.pdf. Retrieved 08 February 2018.
- ↑ "Implementation Plan for The Health Children Initiative" (PDF). Commonwealth of Australia. December 2012. http://www.federalfinancialrelations.gov.au/content/npa/health/_archive/healthy_workers/healthy_children/NSW_IP_2013.pdf. Retrieved 08 February 2018.
- ↑ Lockeridge, A.; Innes-Hughes, C.; O'Hara, B.J. et al. (2015). Munch & Move: Evidence and Evaluation Summary. NSW Ministry of Health. pp. 26. ISBN 9781760003029. https://www.health.nsw.gov.au/heal/Publications/Munch-Move-Evaluation-Summary.pdf. Retrieved 08 February 2018.
- ↑ Bravo, A.; Innes-Hughes, C.; O'Hara, B.J. et al. (2016). Live Life Well @ School: Evidence and Evaluation Summary 2008-2015. NSW Ministry of Health. pp. 31. ISBN 99781760004750. https://www.health.nsw.gov.au/heal/Publications/Munch-Move-Evaluation-Summary.pdf. Retrieved 08 February 2018.
- ↑ Conte, K.P.; Groen, S.; Loblay, V. et al. (2017). "Dynamics behind the scale up of evidence-based obesity prevention: protocol for a multi-site case study of an electronic implementation monitoring system in health promotion practice". Implementation Science 12 (1): 146. doi:10.1186/s13012-017-0686-5. PMC PMC5718021. PMID 29208000. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5718021.
Notes
This presentation is faithful to the original, with only a few minor changes to presentation, spelling, and grammar. We also added PMCID and DOI when they were missing from the original reference.