Book:COVID-19 Testing, Reporting, and Information Management in the Laboratory/Overview of COVID-19 and its challenges/Challenges of managing the disease in the human population
1.3 Challenges of managing the disease in the human population
COVID-19 has presented numerous societal challenges, from supply line interruptions and economic sagging to overwhelmed healthcare systems and civil disorder. However, these are largely the social, economic, and political ripple effects of a disease that has brought with it a set of inherent attributes that make it more difficult to manage in human populations than say the flu.
However, COVID-19 is not the flu, and it is indeed worse in its effects than the flu, contrary to many people's perceptions. Yes, COVID-19 and the flu have some symptom overlap. Yes, COVID-19 and the flu have some transmission type overlap. But from there it diverges. COVID-19 and SARS-CoV-2 is different in that it is more prone to be transmitted to others during the presymptomatic phase. And the body of evidence has grown since early on in the pandemic[1] that SARS-CoV-2 is transmittable predominately via an airborne route[2][3][4][5], though transmission from contaminated surfaced or physical intimacy are also believed possible.[6][7] Hospitalization rates are higher, perhaps up to 10 times higher than the flu, and hospital stays are longer with COVID-19. People are dying more often from COVID-19 too, up to 10 times more often than people stricken with the flu.[8][9][10] And while flu vaccines are largely the norm around the world, and COVID-19 vaccines are gradually becoming more available, those who willing choose to not get the vaccine have a massively higher chance of dying from COVID-19 (as of August 2021, more than 99 percent of all deaths from COVID-19 are found with the unvaccinated[11], compared to some 80% of children who die from the flu while unvaccinated[12]).
Other aspects of the disease that make it difficult to manage include:
- Median incubation period: According to research published in Annals of Internal Medicine, the median (i.e., the central tendency, which is less skewed than average[13]) incubation period is 5.1 days (Note that as new variants arrive, incubation times my change; the delta variant is thought to have an incubation period of four days, for example.[14]), with 97.5% of symptomatic carriers showing symptoms within 11.5 days. The authors found this to be compatible with U.S. government recommendations of monitored 14-day self-quarantines if individuals were at risk of exposure.[15] However, many people continue to not take mask-wearing—and vaccination—seriously, and thus unmasked presymptomatic (and asymptomatic) carriers are thus largely more prone to spreading the virus.[16][17] This has become even more precarious with the highly contagious delta variant, which can be spread even by the vaccinated, highlighting that "measures such as masks and hand hygiene which can reduce transmission are important for everyone, regardless of vaccination status."[18]
- Presymptomatic and asymptomatic virus shedding: As mentioned in the previous point, carriers can be contagious during the presymptomatic phase of the disease, even while remaining symptom-free.[16][17][19][20] (The latest comprehensive research, from August 2021, appears to indicate that 35.1 percent of infected people may go without any recognizable symptoms after infection occurs.[21]) This contagion is a result of what's called viral shedding, when the virus moves from cell to cell following successful reproduction. When the virus is in this state, it can be actively found in a carrier's body fluids, excrement, and other sources. Depending on the virus, the virus can then be introduced to another person via those sources. In the case of COVID-19, the core route of transmission appears to be through the air via aerosolized and other forms of water droplets, though saliva and other bodily constituents pose a transmission hazard due to shedding (see previous bulletpoint). Early in the pandemic, uncertainty about transmission routes of viral shedding, along with mixed messages early on about masks and their effectiveness for COVID-19[22][23][24], caused problems. Today we know that masks and social distancing—when appropriate—are an even stronger necessity to limit community transmission of the disease from presymptomatic and asymptomatic individuals, even for those who are vaccinated.[18]
- Understanding of high viral loads and infectious doses: Respiratory diseases such as influenza, SARS, and MERS see a correlation between the infectious dose amount and the severity of disease symptoms, meaning the higher the infectious dose, the worse the symptoms.[25] Similarly, viral load—a quantification of viral genomic fragments—also tends to correlate with clinical symptoms.[26] However, even with the breakthroughs in COVID research since the start of the pandemic, we are still in the investigative stages of definitively determining if that similarly holds true to COVID-19.[25][27][28] Research early on indicated, for example, there is little difference between the viral load of those with mild or no COVID-19 symptoms and those with more severe symptoms.[25] However, Pujadas et al. suggested a link between high viral load and overall mortality rate.[29] Research later in 2020 has suggested more of a positive correlation between severity of symptoms and viral load[30][31], as has a July 2021 study published in Science.[32] However, more research must be performed to better understand how the viral load infectious dose plays a role in transmission. Given the continued unknowns in this realm, wearing masks and getting vaccinate help minimize exposure and remain the best defense against the worst outcomes of the disease.[25]
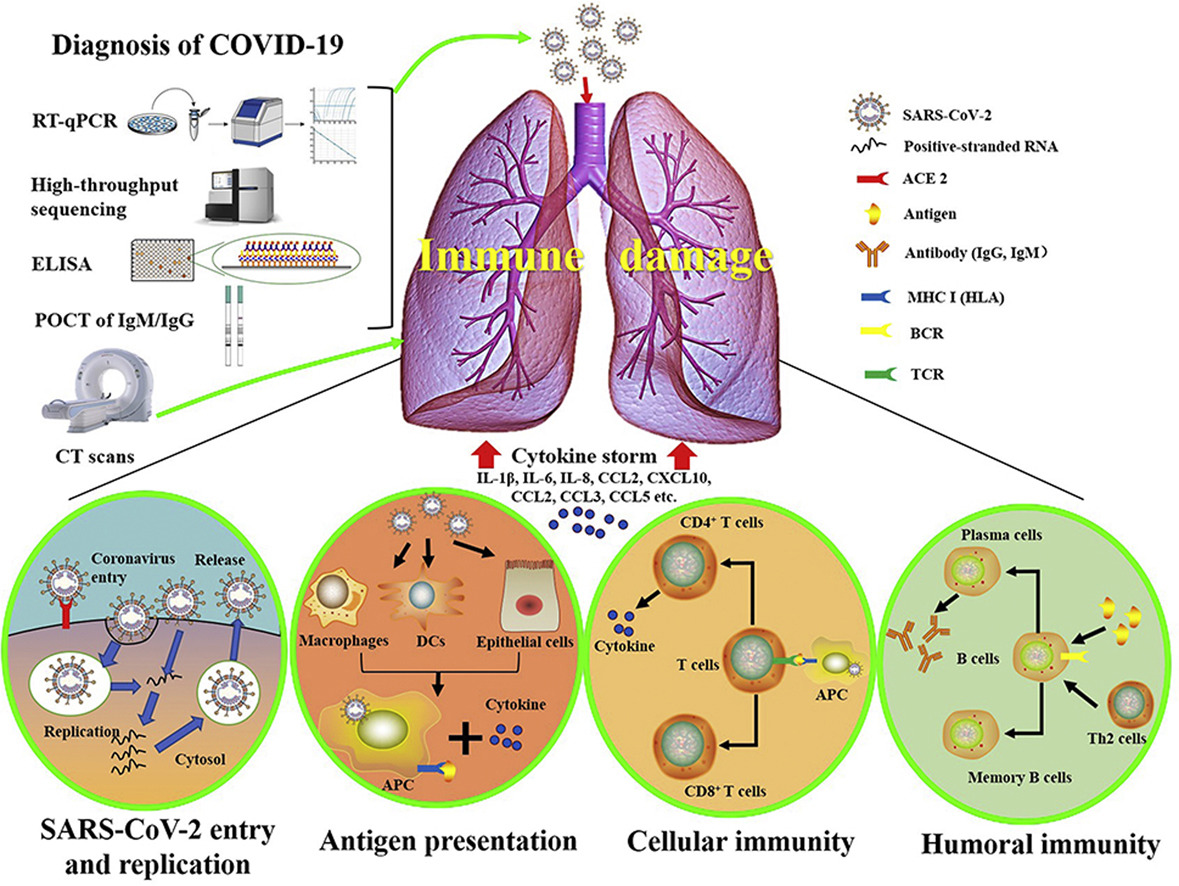
- Cardiovascular issues: Coronaviruses and their accompanying respiratory infections are known to complicate issues of the cardiovascular system, which in turn may "increase the incidence and severity" of infectious diseases such as SARS and COVID-19.[33][34][35] While the exact cardiac effect COVID-19 has on patients is still unknown, suspicion is those with "hypertension, diabetes, and diagnosed cardiovascular disease" may be more prone to having cardiovascular complications from the disease.[36][37] Current thinking is SARS-CoV-2 either attacks heart tissues, causing myocardial dysfunction, or inevitably causes heart failure through a "cytokine storm,"[33][34][36][37][38][39][40], an overproduction of signaling molecules that promote inflammation by white blood cells (leukocytes).[41][42] What's scary is that like the 1918 Spanish flu, SARS, and other epidemics, some otherwise healthy patients' immune responses are entirely overreactive, leading to acute respiratory distress syndrome (ARDS) or heart failure.[40][39][43] Additionally, as the disease has progressed, medical professionals have noted two additional cardiovascular issues. First, an atypical amount of blood clotting has shown up in some infected patients, which may be related to overreactive immune systems, autoantibodies, and underlying health conditions.[44][45] Second, what is being called pediatric multisystem inflammatory syndrome (PMIS) or multisystem inflammatory syndrome in children (MIS-C) has shown up in children after the infection has passed, characterized by inflamed blood vessels and toxic shock syndrome.[46][47][48] While research is ongoing to determine whether these seemingly hyperactive cardiovascular responses are directly linked to the virus[49] or if virus-independent immunopathology is responsible[50], these uncertainties only emphasize the level of difficulty of properly treating COVID-19.
- Other systemic and bodily issues: As the pandemic has progressed, researchers have discovered SARS-CoV-2 appears to negatively impact other organs and systems in the human body, including the renal system, digestive system, endocrine system, neurological system, and even the reproductive system.[40][51][52][53][54] Another bodily issue that appears to remain for a subset of post-recovery COVID-19 patients is fatigue. The University of Minnesota's Center for Infectious Disease Research and Policy reports on an observational study published in PLOS One' that showed more than half of people who recovered from their COVID-19 infection still dealt with the lingering effects of fatigue at a median of 10 weeks after recovery. The study reports no link between the persistent fatigue and severity of symptoms, need for hospitalization, concentration of laboratory biomarkers, and age.[55] These systemic and body issues have added further complication to an already complicated disease, making extended treatment planning difficult. The long-term affects of these and other organ system injuries remains to be fully understood.
- Mental health concerns: The mental health toll of the pandemic is becoming increasingly apparent as it wears on. A June 2020 CDC survey of 5,412 U.S. adults (regardless of infection status) "found that 40.9% of respondents reported 'at least one adverse mental or behavioral health condition,' including depression, anxiety, posttraumatic stress, and substance abuse, with rates that were three to four times the rates one year earlier." More than 10 percent of respondents also indicated they had seriously considered suicide in a time period thirty days prior to responding.[56] From an inability to grieve communally with loved ones, to income loss, increased anxiety, and long periods of social isolation, these increasing numbers are not surprising, particularly in light of research on previous pandemics.[56][57] Without proper treatment, these conditions may worsen into prolonged grief disorder, only exasperating a growing mental health crisis.[56] Further, at least one study suggests that those who contract COVID-19 may be at a greater risk of developing some sort of mental illness within 90 days, including anxiety, depression, and insomnia. This effect may be worse for those who already have a history of mental health illness.[58] Mitigating the effects of these mental health concerns will require further study, greater funding, expanded screening, and improved focus on community methods of dealing with tragedy and loss.[56]
References
- ↑ Achenach, J.; Johnson, C.Y. (29 April 2020). "Studies leave question of ‘airborne’ coronavirus transmission unanswered". The Washington Post. https://www.washingtonpost.com/health/2020/04/29/studies-leave-question-airborne-coronavirus-transmission-unanswered/. Retrieved 01 May 2020.
- ↑ Van Beusekom, M. (6 July 2020). "Global experts: Ignoring airborne COVID spread risky". Center for Infectious Disease Research and Policy. University of Minnesota. https://www.cidrap.umn.edu/news-perspective/2020/07/global-experts-ignoring-airborne-covid-spread-risky. Retrieved 07 July 2020.
- ↑ Ducharme, J. (7 July 2020). "The WHO Says Airborne Coronavirus Transmission Isn't a Big Risk. Scientists Are Pushing Back". Time. https://time.com/5863220/airborne-coronavirus-transmission/. Retrieved 07 July 2020.
- ↑ Penn Medicine (2 August 2020). "COVID-19 Transmission: Droplet or Airborne? Penn Medicine Epidemiologists Issue Statement". Penn Physician Blog. https://www.pennmedicine.org/updates/blogs/penn-physician-blog/2020/august/airborne-droplet-debate-article. Retrieved 23 August 2020.
- ↑ Greenhalgh, T.; Jimenez, J.L.; Prather, K.A. et al. (2021). "Ten scientific reasons in support of airborne transmission of SARS-CoV-2". Lancet 397 (10285): 1603–5. doi:10.1016/S0140-6736(21)00869-2. PMC PMC8049599. PMID 33865497. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8049599.
- ↑ "Science Brief: SARS-CoV-2 and Surface (Fomite) Transmission for Indoor Community Environments". Centers for Disease Control and Prevention. 5 April 2021. https://www.cdc.gov/coronavirus/2019-ncov/more/science-and-research/surface-transmission.html. Retrieved 06 September 2021.
- ↑ Winter, E.; Datil, A. (27 May 2021). "VERIFY: Yes, vaccinated people can transmit COVID-19 through kissing". WUSA9 - Verify. https://www.wusa9.com/article/news/verify/yes-vaccinated-people-can-transmit-covid-through-kissing/536-00d88093-498c-4e58-9db6-331a69618248. Retrieved 06 September 2021.
- ↑ Huang, P. (20 March 2020). "How The Novel Coronavirus And The Flu Are Alike ... And Different". NPR: Goats and Soda. https://www.npr.org/sections/goatsandsoda/2020/03/20/815408287/how-the-novel-coronavirus-and-the-flu-are-alike-and-different. Retrieved 01 April 2020.
- ↑ Resnick, B.; Animashaun, C. (18 March 2020). "Why Covid-19 is worse than the flu, in one chart". Vox. https://www.vox.com/science-and-health/2020/3/18/21184992/coronavirus-covid-19-flu-comparison-chart. Retrieved 01 April 2020.
- ↑ Kumar, V. (27 March 2020). "COVID-19 has been compared to the flu. Experts say that's wrong". ABC News. https://abcnews.go.com/Health/covid-19-compared-flu-experts-wrong/story?id=69779116. Retrieved 01 April 2020.
- ↑ Most, D. (13 August 2021). "Myths vs. Facts: Making Sense of COVID-19 Vaccine Misinformation". The Brink. https://www.bu.edu/articles/2021/myths-vs-facts-covid-19-vaccine/. Retrieved 06 September 2021.
- ↑ "61,000 people died in the worst flu season of the past decade. COVID-19 has killed eight times that many". USAFacts. 29 July 2021. https://usafacts.org/articles/how-many-people-die-flu/. Retrieved 06 September 2021.
- ↑ National Water and Climate Center. "Median vs. Average to Describe Normal". U.S. Department of Agriculture. https://www.wcc.nrcs.usda.gov/normals/median_average.htm. Retrieved 01 April 2020.
- ↑ Kochvar, G.; Shah, A. (16 August 2021). "Delta variant questions answered". Northwest Community Healthcare. https://www.nch.org/news/delta-variant-questions-answered/. Retrieved 06 September 2021.
- ↑ Lauer, S.A.; Grantz, K.H.; Bi, Q. et al. (2020). "The Incubation Period of Coronavirus Disease 2019 (COVID-19) From Publicly Reported Confirmed Cases: Estimation and Application". Annals of Internal Medicine. doi:10.7326/M20-0504. PMC PMC7081172. PMID 32150748. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7081172.
- ↑ 16.0 16.1 Mandavilli, A. (31 March 2020). "Infected but Feeling Fine: The Unwitting Coronavirus Spreaders". The New York Times. https://www.nytimes.com/2020/03/31/health/coronavirus-asymptomatic-transmission.html. Retrieved 01 April 2020.
- ↑ 17.0 17.1 Mock, J. (26 March 2020). "Asymptomatic Carriers Are Fueling the COVID-19 Pandemic. Here’s Why You Don’t Have to Feel Sick to Spread the Disease". Discover. https://www.discovermagazine.com/health/asymptomatic-carriers-are-fueling-the-covid-19-pandemic-heres-why-you-dont. Retrieved 01 April 2020.
- ↑ 18.0 18.1 Subbaraman, N. (2021). "How do vaccinated people spread Delta? What the science says". Nature 596: 327–28. doi:10.1038/d41586-021-02187-1. PMID 34385613.
- ↑ Yuen, K.-S.; Fung, S.-Y.; Chan, C.-P.; Jin, D.-Y. (2020). "SARS-CoV-2 and COVID-19: The most important research questions". Cell & Bioscience 10: 40. doi:10.1186/s13578-020-00404-4. PMC PMC7074995. PMID 32190290. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7074995.
- ↑ Diamond, F. (17 March 2020). "Asymptomatic Carriers of COVID-19 Make It Tough to Target". Infection Control Today. https://www.infectioncontroltoday.com/view/asymptomatic-carriers-covid-19-make-it-tough-target. Retrieved 06 September 2021.
- ↑ Sah, P.; Fitzpatrick, M.C.; Zimmer, C.F. et al. (2021). "Asymptomatic SARS-CoV-2 infection: A systematic review and meta-analysis". PNAS 118 (34): e2109229118. doi:10.1073/pnas.2109229118. PMID 34376550.
- ↑ Greenfieldboyce, N. (28 March 2020). "WHO Reviews 'Current' Evidence On Coronavirus Transmission Through Air". NPR. https://www.npr.org/2020/03/28/823292062/who-reviews-available-evidence-on-coronavirus-transmission-through-air. Retrieved 01 April 2020.
- ↑ Chicago Sun Times Editorial Board (31 March 2020). "Ignore the mixed messages and wear that mask". Chicago Sun Times. https://chicago.suntimes.com/2020/3/31/21200144/coronavirus-covid-19-masks-wear-cdc-pritzker-trump-public-health-virus-face-cough-sneeze. Retrieved 01 April 2020.
- ↑ Mulholland, J. (29 March 2020). "To mask or not to mask: mixed messages in a time of crisis". RFI. http://www.rfi.fr/en/international/20200329-to-mask-or-not-to-mask-mixed-messages-in-a-time-of-coronavirus-crisis-france-covid-19-spread-droplets. Retrieved 01 April 2020.
- ↑ 25.0 25.1 25.2 25.3 Geddes, L. (27 March 2020). "Does a high viral load or infectious dose make covid-19 worse?". New Scientist. https://www.newscientist.com/article/2238819-does-a-high-viral-load-or-infectious-dose-make-covid-19-worse/. Retrieved 01 April 2020.
- ↑ Hijano, D.R.; Brazelton de Cardenas, J.; Maron, G. et al. (2019). "Clinical correlation of influenza and respiratory syncytial virus load measured by digital PCR". PLoS One 14 (9): e0220908. doi:10.1371/journal.pone.0220908. PMC PMC6720028. PMID 31479459. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6720028.
- ↑ Liu, Y.; Yan, L.-M.; Wan, L. et al. (2020). "Viral dynamics in mild and severe cases of COVID-19". The Lancet Infectious Diseases. doi:10.1016/S1473-3099(20)30232-2. PMID 32199493.
- ↑ Joynt, G.M.; Wu, W.K.K. (2020). "Understanding COVID-19: what does viral RNA load really mean?". The Lancet Infectious Diseases. doi:10.1016/S1473-3099(20)30237-1.
- ↑ Pujadas, E.; Chaudhry, F.; McBride, R. et al. (2020). "SARS-CoV-2 viral load predicts COVID-19 mortality". The Lancet Respiratory Medicine. doi:10.1016/S2213-2600(20)30354-4.
- ↑ Fajnzylber, J.; Regan, J.; Coxen, K. et al. (2020). "SARS-CoV-2 viral load is associated with increased disease severity and mortality". Nature Communications 11: 5493. doi:10.1038/s41467-020-19057-5. PMC PMC7603483. PMID 33127906. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7603483.
- ↑ "SARS-Cov-2 Viral Load as an Indicator for COVID-19 Patients’ Hospital Stay". medRxiv. 2020. doi:10.1101/2020.11.04.20226365.
- ↑ Jones, T.C.; Biele, G.; Mühlemann, B. et al. (2021). "Estimating infectiousness throughout SARS-CoV-2 infection course". Science 373 (6551): abi5273. doi:10.1126/science.abi5273. PMID 34035154.
- ↑ 33.0 33.1 Madjid, M.; Safavi-Naeini, P.; Solomon, S.D. (2020). "Potential Effects of Coronaviruses on the Cardiovascular System". JAMA Cardiology. doi:10.1001/jamacardio.2020.1286. PMID 32219363.
- ↑ 34.0 34.1 Xiong, T.-Y.; Redwood, S.; Prendergast, B.; Chen, M. (2020). "Coronaviruses and the cardiovascular system: acute and long-term implications". European Heart Journal: ehaa231. doi:10.1093/eurheartj/ehaa231. PMID 32186331.
- ↑ Driggin, E.; Madhavan, M.V.; Bikdeli, B. et al. (2020). "Cardiovascular Considerations for Patients, Health Care Workers, and Health Systems During the Coronavirus Disease 2019 (COVID-19) Pandemic". Journal of the American College of Cardiology. doi:10.1016/j.jacc.2020.03.031. PMID 32201335.
- ↑ 36.0 36.1 Otto, M.A. (26 March 2020). "Cardiac symptoms can be first sign of COVID-19". The Hospitalist. https://www.the-hospitalist.org/hospitalist/article/219645/coronavirus-updates/cardiac-symptoms-can-be-first-sign-covid-19. Retrieved 01 April 2020.
- ↑ 37.0 37.1 Clerkin, K.J.; Fried, J.A.; Raikhelkar, J. et al. (2020). "Coronavirus Disease 2019 (COVID-19) and Cardiovascular Disease". Circulation. doi:10.1161/CIRCULATIONAHA.120.046941. PMID 32200663.
- ↑ Mehta, P.; McAuley, D.F.; Brown, M. et al. (2020). "COVID-19: Consider cytokine storm syndromes and immunosuppression". The Lancet 395 (10229): P1033–34. doi:10.1016/S0140-6736(20)30628-0. PMID 32192578.
- ↑ 39.0 39.1 Mandavilli, A. (1 April 2020). "The Coronavirus Patients Betrayed by Their Own Immune Systems". The New York Times. https://www.nytimes.com/2020/04/01/health/coronavirus-cytokine-storm-immune-system.html. Retrieved 01 April 2020.
- ↑ 40.0 40.1 40.2 Weidmann, M.D.; Otori, J.; Rai, A.J. (2020). "Laboratory Biomarkers in the Management of Patients With COVID-19". American Journal of Clinical Pathology: aqaa205. doi:10.1093/ajcp/aqaa205. PMID 33107558.
- ↑ Tisoncik, J.R.; Korth, M.J.; Simmons, C.P. et al. (2012). "Into the eye of the cytokine storm". Microbiology and Molecular Biology Reviews 76 (1): 16–32. doi:10.1128/MMBR.05015-11. PMC PMC3294426. PMID 22390970. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3294426.
- ↑ Yang, L.; Xie, X.; Tu, Z. et al. (2021). "The signal pathways and treatment of cytokine storm in COVID-19". Signal Transduction and Targeted Therapy 6: 255. doi:10.1038/s41392-021-00679-0. PMC PMC8261820. PMID 34234112. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8261820.
- ↑ Basilio, P. (26 March 2020). "A new potential risk of COVID-19: Sudden cardiac death". MDLinx. https://www.mdlinx.com/article/a-new-potential-risk-of-covid-19-sudden-cardiac-death/3z05mHtQN0PL1EdhlWltmH. Retrieved 06 September 2021.
- ↑ Rettner, R. (23 April 2020). "Mysterious blood clots in COVID-19 patients have doctors alarmed". LiveScience. https://www.livescience.com/coronavirus-blood-clots.html. Retrieved 28 April 2020.
- ↑ Hampton, T. (2021). "Autoantibodies May Drive COVID-19 Blood Clots". JAMA 325 (5): 425. doi:10.1001/jama.2020.25699. PMID 33528515.
- ↑ Moyer, M.W. (19 May 2020). "What We Know About the Covid-Related Syndrome Affecting Children". The New York Times. https://www.nytimes.com/2020/05/19/parenting/pmis-coronavirus-children.html. Retrieved 19 May 2020.
- ↑ Fischer, K. (18 May 2020). "What to Know About PMIS, the COVID-19-Linked Syndrome Affecting Children". Healthline. https://www.healthline.com/health-news/what-to-know-pmis-syndrome-linked-to-covid-19-affects-children. Retrieved 19 May 2020.
- ↑ MacMillan, C. (14 July 2021). "Researchers Continue to Find Clues About MIS-C". Yale Medicine. Yale University. https://www.yalemedicine.org/news/multisystem-inflammatory-syndrome-in-children-misc-covid-kids. Retrieved 06 September 2021.
- ↑ Manne, B.K.; Denorme, F.; Middleton, E.A. et al. (2020). "Platelet Gene Expression and Function in COVID-19 Patients". Blood: blood.2020007214. doi:10.1182/blood.2020007214.
- ↑ Dorward, D.A.; Russell, C.D.; Um, I.H. et al. (2020). "Tissue-specific tolerance in fatal Covid-19". medRxiv. doi:10.1101/2020.07.02.20145003.
- ↑ Centers for Disease Control and Preventions (22 February 2021). "Symptoms of Coronavirus". Centers for Disease Control and Preventions. https://www.cdc.gov/coronavirus/2019-ncov/symptoms-testing/symptoms.html. Retrieved 06 September 2021.
- ↑ Mayo Clinic Staff (7 October 2020). "COVID-19 (coronavirus): Long-term effects". Mayo Clinic. https://www.mayoclinic.org/diseases-conditions/coronavirus/in-depth/coronavirus-long-term-effects/art-20490351. Retrieved 12 November 2020.
- ↑ Budson, A.E. (8 October 2020). "The hidden long-term cognitive effects of COVID-19". Harvard Health Blog. https://www.health.harvard.edu/blog/the-hidden-long-term-cognitive-effects-of-covid-2020100821133. Retrieved 12 November 2020.
- ↑ Ma, C.; Cong, Y.; Zhang, H. (2020). "COVID-19 and the Digestive System". American Journal of Gastroenterology 115 (7): 1003–6. doi:10.14309/ajg.0000000000000691. PMC PMC7273952. PMID 32618648. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7273952.
- ↑ Van Beusekom, M. (11 November 2020). "Half of recovered COVID-19 patients report lingering fatigue". CUDRAP News & Perspective. University of Minnesota. https://www.cidrap.umn.edu/news-perspective/2020/11/half-recovered-covid-19-patients-report-lingering-fatigue. Retrieved 18 November 2020.
- ↑ 56.0 56.1 56.2 56.3 Simon, N.M.; Saxe, G.N.; Marmar, C.R. (2020). "Mental Health Disorders Related to COVID-19–Related Deaths". JAMA 324 (15): 1493–94. doi:10.1001/jama.2020.19632. PMID 33044510.
- ↑ Savage, M. (28 October 2020). "Coronavirus: The possible long-term mental health impacts". BBC Worklife. https://www.bbc.com/worklife/article/20201021-coronavirus-the-possible-long-term-mental-health-impacts. Retrieved 18 November 2020.
- ↑ Kelland, K. (9 November 2020). "Study Shows COVID-19 Patients at Greater Risk of Mental Health Problems". Insurance Journal. https://www.insurancejournal.com/news/international/2020/11/09/590113.htm. Retrieved 18 November 2020.
Citation information for this chapter
Chapter: 1. Overview of COVID-19 and its challenges
Edition: Fall 2021
Title: COVID-19 Testing, Reporting, and Information Management in the Laboratory
Author for citation: Shawn E. Douglas
License for content: Creative Commons Attribution-ShareAlike 4.0 International
Publication date: September 2021









