Difference between revisions of "Journal:Development of a core competency framework for clinical informatics"
Shawndouglas (talk | contribs) (Saving and adding more.) |
Shawndouglas (talk | contribs) (Saving and adding more.) |
||
| Line 169: | Line 169: | ||
Social workers, the social care sector tends to notice these things, if they feel it’s too contextualized within healthcare than social care ... And you have some healthcare professionals who really lean more towards working in the community for instance. So their roles overlap much more with their social care, social work side of the system. And so it would be helpful for that to be reflected as well. – P8</blockquote> | Social workers, the social care sector tends to notice these things, if they feel it’s too contextualized within healthcare than social care ... And you have some healthcare professionals who really lean more towards working in the community for instance. So their roles overlap much more with their social care, social work side of the system. And so it would be helpful for that to be reflected as well. – P8</blockquote> | ||
'''Missing competency''' | |||
Table 3 summarizes what participants viewed as missing competencies. | |||
{| | |||
| STYLE="vertical-align:top;"| | |||
{| class="wikitable" border="1" cellpadding="5" cellspacing="0" width="60%" | |||
|- | |||
| style="background-color:white; padding-left:10px; padding-right:10px;" colspan="2"|'''Table 3.''' Summary of missing competencies identified by participants | |||
|- | |||
! style="background-color:#dddddd; padding-left:10px; padding-right:10px;"|Participant | |||
! style="background-color:#dddddd; padding-left:10px; padding-right:10px;"|Missing competency | |||
|- | |||
| style="background-color:white; padding-left:10px; padding-right:10px;"|P1 | |||
| style="background-color:white; padding-left:10px; padding-right:10px;"|1. Choosing between types of hardware and technology.<br />2. How data is transmitted between systems.<br />3. Accessing ethical and legislative requirements. | |||
|- | |||
| style="background-color:white; padding-left:10px; padding-right:10px;"|P4 | |||
| style="background-color:white; padding-left:10px; padding-right:10px;"|1. How to access and use evidence bases (ie, collating evidence for a start-up).<br />2. Communication as part of change management (e.g., workshops, comms teams, weekly meetings, and teaching sessions).<br />3. Ethics and clinical safety. | |||
|- | |||
| style="background-color:white; padding-left:10px; padding-right:10px;"|P5 | |||
| style="background-color:white; padding-left:10px; padding-right:10px;"|1. More on governance and regulatory frameworks.<br />2. Validation and verification of software.<br />3. Audit cycles.<br />4. Presenting data visually to patients (ie, infographics).<br />5. Communicating with stakeholders and getting management buy-in. | |||
|- | |||
| style="background-color:white; padding-left:10px; padding-right:10px;"|P6 | |||
| style="background-color:white; padding-left:10px; padding-right:10px;"|1. Agile project management. | |||
|- | |||
| style="background-color:white; padding-left:10px; padding-right:10px;"|P7 | |||
| style="background-color:white; padding-left:10px; padding-right:10px;"|1. Postgraduate teaching and supervising. | |||
|- | |||
| style="background-color:white; padding-left:10px; padding-right:10px;"|P8 | |||
| style="background-color:white; padding-left:10px; padding-right:10px;"|1. Understanding integration between systems (i.e., clinical and social care systems).<br />2. Ethical decision-making. | |||
|- | |||
| style="background-color:white; padding-left:10px; padding-right:10px;"|P11 | |||
| style="background-color:white; padding-left:10px; padding-right:10px;"|1. Understanding more about others roles. | |||
|- | |||
| style="background-color:white; padding-left:10px; padding-right:10px;"|P12 | |||
| style="background-color:white; padding-left:10px; padding-right:10px;"|1. Decision-making should have its own domain.<br />2. Action behavioral change. | |||
|- | |||
| style="background-color:white; padding-left:10px; padding-right:10px;"|P14 | |||
| style="background-color:white; padding-left:10px; padding-right:10px;"|1. Leadership resilience. | |||
|- | |||
| style="background-color:white; padding-left:10px; padding-right:10px;"|P15 | |||
| style="background-color:white; padding-left:10px; padding-right:10px;"|1. Clinical improvement as its own section (research and evaluation of what we are doing). | |||
|- | |||
|} | |||
|} | |||
Revision as of 21:21, 13 August 2021
| Full article title | Development of a core competency framework for clinical informatics |
|---|---|
| Journal | BMJ Health & Care Informatics |
| Author(s) | Davies, Alan; Mueller, Julia; Hassey, Alan; Moulton, Georgina |
| Author affiliation(s) | University of Manchester, University of Cambridge, The Faculty of Clinical Informatics, Health Data Research UK |
| Primary contact | alan dot davies at ucl dot ac dot uk |
| Year published | 2021 |
| Volume and issue | 28(1) |
| Article # | e100356 |
| DOI | 10.1136/bmjhci-2021-100356 |
| ISSN | 2632-1009 |
| Distribution license | Creative Commons Attribution-NonCommercial 4.0 International |
| Website | https://informatics.bmj.com/content/28/1/e100356 |
| Download | https://informatics.bmj.com/content/bmjhci/28/1/e100356.full.pdf (PDF) |
|
|
This article should not be considered complete until this message box has been removed. This is a work in progress. |
Abstract
Objectives: Up to this point, there has not been a national core competency framework for clinical informatics in the U.K. Here we report on the final two iterations of work carried out towards the formation of a national core competency framework. This follows an initial systematic literature review of existing skills and competencies and a job listing analysis.
Methods: An iterative approach was applied to framework development. Using a mixed-methods design, we carried out semi-structured interviews with participants involved in informatics (n = 15). The framework was updated based on the interview findings and was subsequently distributed as part of a bespoke online digital survey for wider participation (n = 87). The final version of the framework is based on the findings of the survey.
Results: Over 102 people reviewed the framework as part of the interview or survey process. This led to a final core competency framework containing six primary domains with 36 subdomains containing 111 individual competencies.
Conclusions: An iterative mixed-methods approach for competency development involving the target community was appropriate for development of the competency framework. There is some contention around the depth of technical competencies required. Care is also needed to avoid professional burnout, as clinicians and healthcare practitioners already have clinical competencies to maintain. Therefore, how the framework is applied in practice and how practitioners meet the competencies requires careful consideration.
Introduction
The healthcare sector in many countries is facing increasing demand as people live longer and healthier lives.[1] The public’s expectation of healthcare is also increasing and is tempered by various financial constraints. The healthcare sector has lagged behind other sectors regarding its adoption and use of digital technology. In the U.K., the Topol review was carried out to assess how the healthcare workforce can be prepared for the digital future. The review makes many recommendations on the use of genomics technology, robotics, artificial intelligence (AI), and digital medicine, including the training and education of healthcare professionals in such areas.[1] At the cutting edge of this digital upskilling of the workforce are informaticians from clinical, health, and social care disciplines.
The American Medical Informatics Association (AMIA) defines clinical informatics as "the application of informatics and information technology to deliver healthcare services."[2] The U.K. Faculty of Clinical Informatics (FCI) defines a clinical informatician as someone who "uses their clinical knowledge and experience of informatics concepts, methods, and tools to promote patient and population care that is person-centred, ethical, safe, effective, efficient, timely, and equitable."[3]
As of yet there are no U.K.-based overarching competency frameworks aimed at multiple informatics disciplines. Existing frameworks tend to focus on specific domains such as nursing informatics or bioinformatics.[4] The U.K. FCI was created to provide support for clinical informaticians, including those with clinical roles in the health and social care domains applying informatics in practice. It is the intention of the FCI to provide and accredit competencies for informaticians. This includes accreditation of the U.K.’s National Health Service (NHS) Digital Academy program which aims to create digital leaders for the digital transformation of the NHS. The present study forms part of a program commissioned by the FCI to create a national competency framework for clinical informaticians in the U.K.
Competency describes the behaviors, characteristics, skills, attitudes, and knowledge application used to successfully achieve something. Competence therefore is the achievement of a single competency or multiple competencies. A core competency framework describes the essential set of competencies required to achieve competence in a specific area. Many competency frameworks aimed at various clinical informatics disciplines currently exist, such as the ELIXIR (European Life-science Infrastructure for Biological Information) and TIGER (Technology Informatics Guiding Education Reform) frameworks for bioinformaticians and nurses. This paper reports on the methods used to generate and refine the U.K. FCI’s Core Competency Framework (CCF), which covers the core competencies required to develop clinical informaticians’ professional competencies, and to provide a process for the FCI to provide accreditation for training and education programs and individual clinical informaticians.[5]
Background
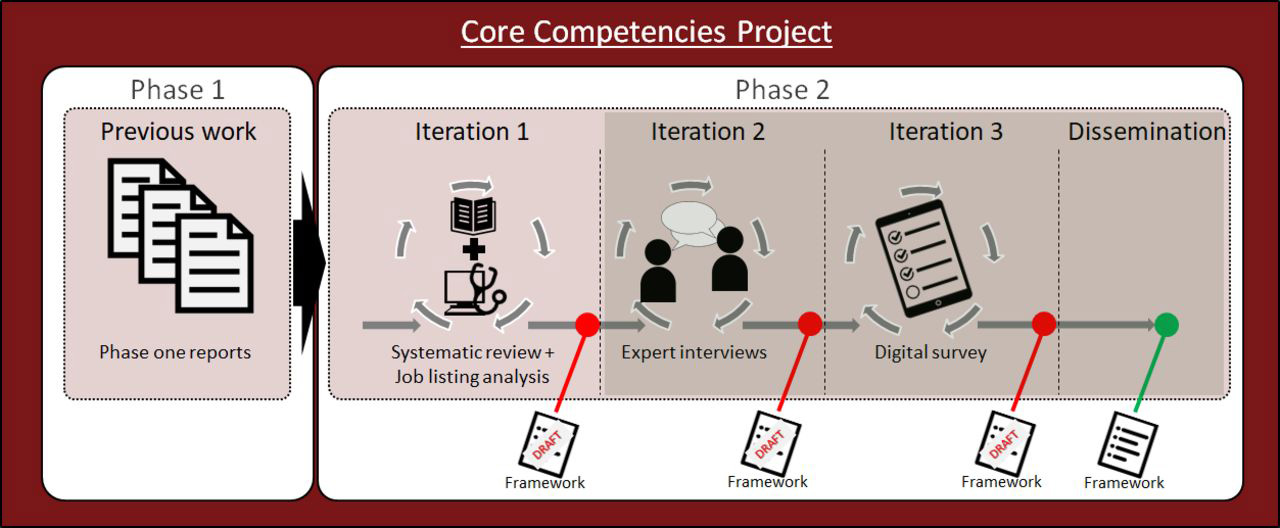
The Core Competencies Project spanned two primary phases. The first part of the work explored the definition of the professional attributes of a clinical informatician. The FCI carried out the first phase of the work (Figure 1), which consisted of three reports based on (1) discovery[6], (2) validation[7], and (3) consultation around the output competences of a clinical informatician.[3] This included defining clinical informatics, clinical informaticians, inclusivity, professional boundaries, and the functional domains (scope) of clinical informatics practice. This work was carried out using qualitative methods (e.g., interviews) with the faculty’s membership. The second phase (reported in this paper) involved an iterative process consisting of three separate iterations. The first iteration involved the combination of findings from both academia and industry in the form of an analysis of over 50 informatics job postings and a systematic literature review which explored the commonality of informatics competencies across different clinical informatics domains (such as medicine, nursing, pharmacy).[4] Following synthesis of this information, an initial draft competency framework was generated, which was then presented to 15 informatics experts in one-to-one semi-structured interviews and adapted following feedback. The amended version was presented for wider evaluation through a digital survey with 87 participants. In light of the survey results, the final version of the competency framework[5] was updated and disseminated publicly on the FCI’s website.
|
Figure 1 provides an overview of the iterative steps followed to create the final core competency framework. This paper reports on the interviews and survey (iterations 2 and 3 of phase two). The principle research questions were:
- RQ1: Was the chosen mixed-methods approach appropriate for generating a core competency framework?
- RQ2: How do participants feel the framework should be applied and to whom?
- RQ3: What competencies were considered "core" and how do they fit in with an evolving profession?
Iteration 1: Interviews
Methods
Semi-structured interviews were carried out with participants (n = 15) involved in various aspects of informatics. Participants were sent a copy of the interview schedule (see Box 2 in the supplied supplementary material) and the framework prior to the agreed interview date. Due to the COVID-19 lockdown, the interviews were carried out online using Zoom and audio recorded. Transcribed interviews were analyzed using framework analysis.[8] Framework analysis involves five stages consisting of familiarization with the data, identification of the thematic framework, indexing, charting, and mapping/interpretation. We followed the Standards for Reporting Qualitative Research (SRQR) guidelines.[9] The interview quotes were then stratified into themes by one researcher, and the quotes were independently matched to the primary themes by another. The percentage agreement between both researchers was 85.6%, with an unweighted Cohen’s kappa showing substantial agreement (κ = 0.67).
The sample
A purposive sample was obtained through the FCI, who sought to contact a wide variety of its members and associates with different professional backgrounds. Participants were from a broad set of backgrounds (Table 1). Participants were involved in informatics at various levels, from being the sole informatician in an organization through to Chief Clinical Information Officers (CCIOs) and digital leads. We omit the current roles of participants to maintain anonymity. Sectors of employment included the NHS, adult social care, and the prison system. Age and other demographic details were not requested. The clinical backgrounds were also varied and included general practice, urological surgery, pathology, and oncology. Nurses represented multiple clinical areas across their careers in both the NHS and private sector (including nursing homes).
| ||||||||||||||||||||
Researcher characteristics and reflexivity
Following the SRQR guidelines[9], details of the researchers' characteristics and personal attributes that may influence the research are detailed. Alan Davies (AD) has a background in computer science (PhD) and nursing science (BSc). AD works as a senior lecturer in health informatics and health data sciences and was previously a software engineer/data scientist in industry and a former cardiac nurse. AD did not personally know any of the interviewees that took part in the study, with the exception of one lecturer whom he knows in a professional capacity. AD’s research paradigm is situated in post-positivism. Julia Mueller (JM) has a background in health psychology (MSc, PhD). JM formerly worked as a lecturer in healthcare sciences teaching a course unit on digital public health, and currently works as a research associate in behavioral weight management. JM did not personally know any of the interviewees. JM’s research paradigm is situated in constructivism.
Results
A total of eight hours and 25 minutes (M = 33.66, SD = 12.28) of interview data were generated. Given the nature and topic of the interviews the results are reported in two main ways. The first set of results pertains to the required changes to the composition of the framework and to specific areas such as a specified competency. This does not require any interpretive themes and is reported descriptively. The second set of results uses framework analysis to identify themes around the potential application of the framework, who it is for, and how the participants see the informatics profession changing in the future.
Requested changes to the framework
Table 2 provides an overview of the suggested changes to the framework, broken down by topic and subtopic. This shows how many participants mentioned this topic and how many times.
| |||||||||||||||||||||||||||||||||
Framework composition
Language and terminology
It was mentioned (n = 2) that the wording should make specific reference to "social care" rather than just "healthcare":
... you just get people looking at it, and thinking, that doesn’t apply to me. And then they never revisit it. So, it’s that first impression of appearing as welcoming as they actually are, and showing from within the competencies, that they recognize that it’s not about a job title, it’s about the roles you are doing. – P2 Social workers, the social care sector tends to notice these things, if they feel it’s too contextualized within healthcare than social care ... And you have some healthcare professionals who really lean more towards working in the community for instance. So their roles overlap much more with their social care, social work side of the system. And so it would be helpful for that to be reflected as well. – P8
Missing competency
Table 3 summarizes what participants viewed as missing competencies.
| ||||||||||||||||||||||||
Supplemental material
Supplementary material 1 (PDF)
References
- ↑ 1.0 1.1 Health Education England (2019). "The Topol Review – Preparing the healthcare workforce to deliver the digital future". NHS. https://topol.hee.nhs.uk/.
- ↑ American Medical Informatics Association. "Informatics: Research and Practice". American Medical Informatics Association. https://amia.org/about-amia/why-informatics/informatics-research-and-practice#:~:text=Clinical%20Informatics-,Clinical%20Informatics%20is%20the%20application%20of%20informatics%20and%20information%20technology,clinical%20informatics%20and%20operational%20informatics.&text=Clinical%20Informatics. Retrieved 02 September 2020.
- ↑ 3.0 3.1 Hassey, A.; Jidkov, L.; Williams, J. (2020). "Report C: Consultation stage - Consultation Exercise and Output Competences for a Clinical Informatician". Core Competencies Project - Phase 1 Final Summary Report. p. 22. https://facultyofclinicalinformatics.org.uk/core-competencies-phase1.
- ↑ 4.0 4.1 Davies, Alan; Mueller, Julia; Moulton, Georgina (1 September 2020). "Core competencies for clinical informaticians: A systematic review". International Journal of Medical Informatics 141: 104237. doi:10.1016/j.ijmedinf.2020.104237. ISSN 1872-8243. PMID 32771960. https://pubmed.ncbi.nlm.nih.gov/32771960.
- ↑ 5.0 5.1 Moulton, Georgina; Davies, Alan; Mueller, Julia (22 July 2020) (in en). Protocol: Development of core competencies for Clinical Informatics in the UK. doi:10.5281/ZENODO.3956373. https://zenodo.org/record/3956373.
- ↑ Quinn, N.; Hassey, A.; Jidkov, L. (2020). "Report A: Discovery stage: Develop and Define the Professional Attributes of a Clinical Informatician – Final Report". Core Competencies Project - Phase 1 Final Summary Report. https://facultyofclinicalinformatics.org.uk/core-competencies-phase1.
- ↑ Hassey, A.; Jidkov, L.; Williams, J. (2020). "Report B: Validation stage - Validation Study and draft Output Competences for a Clinical Informatician". Core Competencies Project - Phase 1 Final Summary Report. https://facultyofclinicalinformatics.org.uk/core-competencies-phase1.
- ↑ Ritchie, J.; Spencer, L. (1994). "Qualitative data analysis for applied policy research". In Bryman, A.; Burgess, B. (in English). Analyzing Qualitative Data. Routledge. pp. 173–94. ISBN 978-0-203-41308-1. OCLC 1020495928. https://www.worldcat.org/title/mediawiki/oclc/1020495928.
- ↑ 9.0 9.1 O'Brien, Bridget C.; Harris, Ilene B.; Beckman, Thomas J.; Reed, Darcy A.; Cook, David A. (1 September 2014). "Standards for reporting qualitative research: a synthesis of recommendations". Academic Medicine: Journal of the Association of American Medical Colleges 89 (9): 1245–1251. doi:10.1097/ACM.0000000000000388. ISSN 1938-808X. PMID 24979285. https://pubmed.ncbi.nlm.nih.gov/24979285.
Notes
This presentation is faithful to the original, with only a few minor changes to presentation. A few grammar and spelling errors were also corrected. In some cases important information was missing from the references, and that information was added.