Journal:Management of post-analytical processes in the clinical laboratory according to ISO 15189:2012: Considerations about the management of clinical samples, ensuring quality of post-analytical processes and laboratory information management
| Full article title | Management of post-analytical processes in the clinical laboratory according to ISO 15189:2012: Considerations about the management of clinical samples, ensuring quality of post-analytical processes and laboratory information management |
|---|---|
| Journal | Advances in Laboratory Medicine |
| Author(s) | Yeste, Mᵃ L.L.; Mas, Antonia R.P.; Muñoz, Leonor G.; Álvarez, Silvia I.; García, Fernando M.; Font, Aurora B.; Gómez, Natalia F.P.; Gancedo, Lorena S.; Álvarez, Ana G.; Andreu, Francisco A.B.; Rodríguez, Mᵃ P.C.; Domínguez, Luisa Á. |
| Author affiliation(s) | CATLAB, Hospital Universitari Son Espases, Hospital de la Santa Creu y Sant Pau, Hospital Universitario Miguel Servet, Germans Trias i Pujols Universitary Hospital, Hospital Universitari de Bellvitge, Hospital Universitario de la Princesa, Institute of Oncologic and Molecular Oncology, Hospital Clínico San Carlos, Hospital Universitario Puerta de Hierro, Laboratory Accreditation Board of the Spanish Society of Laboratory Medicine |
| Primary contact | Email: llopez at catlab dot cat |
| Year published | 2021 |
| Volume and issue | 2(3) |
| Page(s) | 373-380 |
| DOI | 10.1515/almed-2021-0044 |
| ISSN | 2628-491X |
| Distribution license | Creative Commons Attribution 4.0 International |
| Website | https://www.degruyter.com/document/doi/10.1515/almed-2021-0044/html |
| Download | https://www.degruyter.com/document/doi/10.1515/almed-2021-0044/pdf (PDF) |
|
|
This article should be considered a work in progress and incomplete. Consider this article incomplete until this notice is removed. |
Abstract
ISO 15189:2012 Medical laboratories — Requirements for quality and competence establishes the requirements for clinical specimen management, ensuring the quality of processes and laboratory information management. ENAC (Entidad Nacional de Acreditación), the sole accreditation authority in Spain, established the requirements for the authorized use of the ISO 15189 accreditation label in reports issued by accredited laboratories. These recommendations are applicable to the lab's post-analytical processes and the professionals involved. The standard requires laboratories to define and document the duration and conditions of specimen retention. Laboratories are also required to design an internal quality control scheme to verify whether post-analytical activities attain the expected standards. Information management requirements are also established, and laboratories are required to design a contingency plan to ensure the communication of laboratory results. Instructions are finally provided about the correct use of the accreditation label in laboratory reports. A range of nations and scientific societies support clinical laboratories being required to obtain accreditation. With ISO 15189 being the most specific standard for demonstrating technical performance, a clear understanding of its requirements is essential for proper implementation.
Keywords: accreditation, clinical laboratory, ISO 15189 standard, laboratory information system, post-analytical
Introduction
Clinical laboratories increasingly devote more efforts to improving their methodological and communication skills to help physicians in the interpretation of test results and improve patient outcomes. This type of quality control is found in UNE EN ISO 15189:2013 Medical laboratories — Requirements for quality and competence (ISO 15189:2012, Corrected version 2014-08-15; hereinafter, the ISO 15189 standard), which addresses the revision, reporting, and release of clinical test results[1], as well as other requirements for post-analytical processes. These requirements also address specimen storage, retention, and disposal; the inclusion of post-analytical processes in laboratory quality assurance and continuous improvement; laboratory information management; and the need for a contingency plan that ensures the communication of test results in any scenario.[2][3] ISO 15189 is based on laboratory best practices and employs the information obtained from the lab's quality management system to generate corrective and improvement actions.
ISO 15189 also establishes a set of requirements for laboratories to implement effective methods for the detection and classification of post-analytical errors and the incorporation of information systems and standard operating procedures (SOPs) aimed at reducing errors.[4] Special emphasis is placed on the communication of results, laboratory information management, and risk management. The standard also requires that a contingency plan is designed.
Additionally, and considering that the use of the ENAC (Entidad Nacional de Acreditación) label in laboratory reports is the way Spanish laboratories demonstrate that they comply with accreditation requirements, it is important all accredited laboratories pay attention to the ENAC document CEA-ENAC-01 Requirements for the use of the ENAC label and reference of certification, which establishes the requirements for ENAC and ISO 15189 accreditation label use.[5] However, these ENAC recommendations do not extend the standard and should be considered complementary information that facilitates its interpretation and implementation. The scope of application is the staff involved in post-analytical processes in the clinical laboratory.
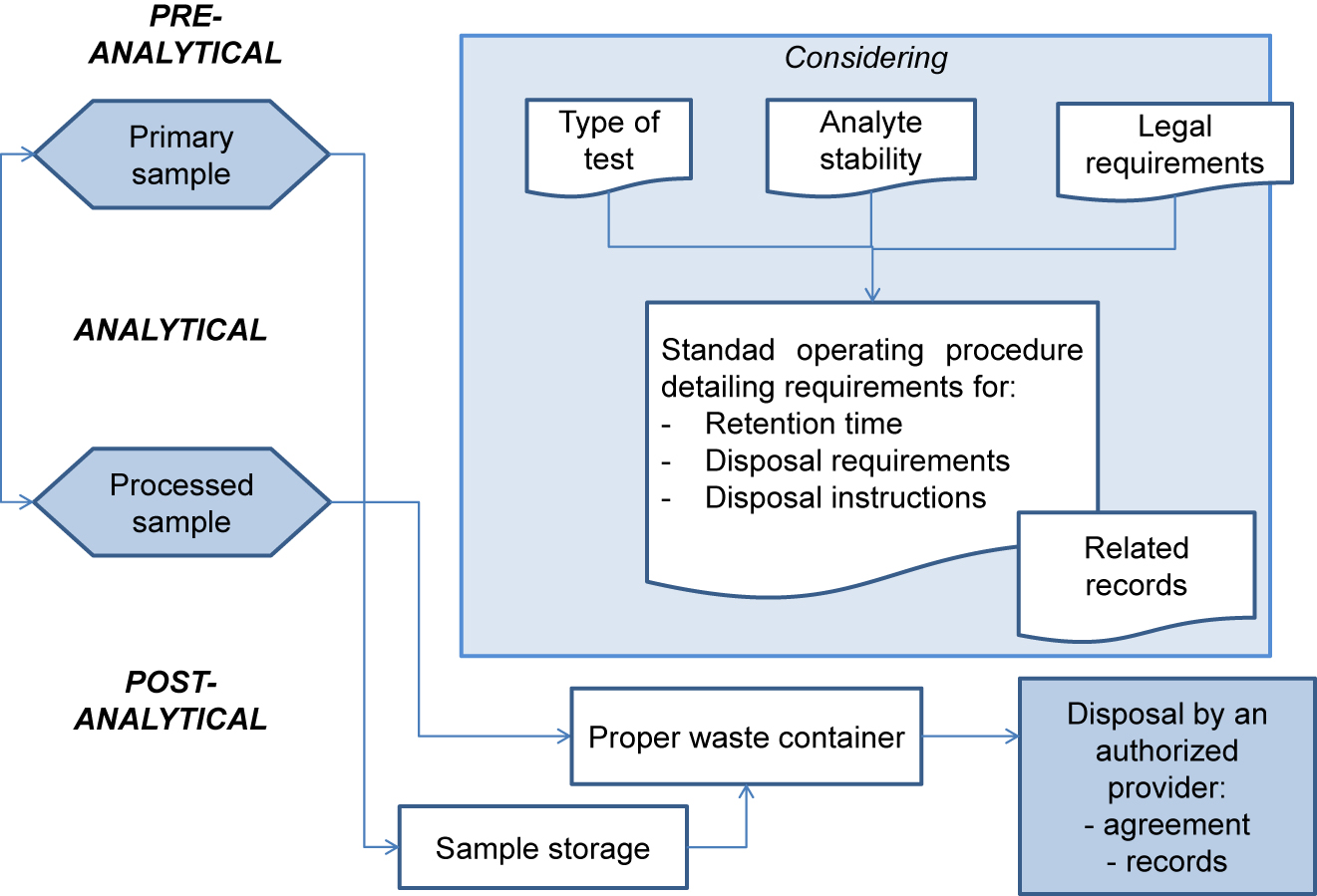
Specimen storage, retention, and disposal
ISO 15189 requires that the laboratory define and document the duration of specimen retention, as well as specimen storage and discard conditions. The standard operating procedure should specify the duration of specimen retention and storage conditions, which will be defined according to the nature and stability of each analyte[6] and the applicable legal requirements (see Figure 1). The duration of specimen storage may be extended by legal requirements associated with some types of studies (e.g., histological analyses, gene testing, pediatric studies).
|
Access to archive specimens must be restricted. Easy specimen traceability and location for retrieval must be ensured (for additional testing, result verification, and/or legal requirement, among others). Therefore, it is recommended that the date and person responsible for specimen retrieval be recorded, which is essential in case it is required by law.
The procedure for disposal of clinical specimens and consumables must be documented by the laboratory. It is laboratory’s responsibility to comply with the laws and regulations in relation to the prevention of occupation hazards, even though waste disposal is performed by an authorized external supplier.
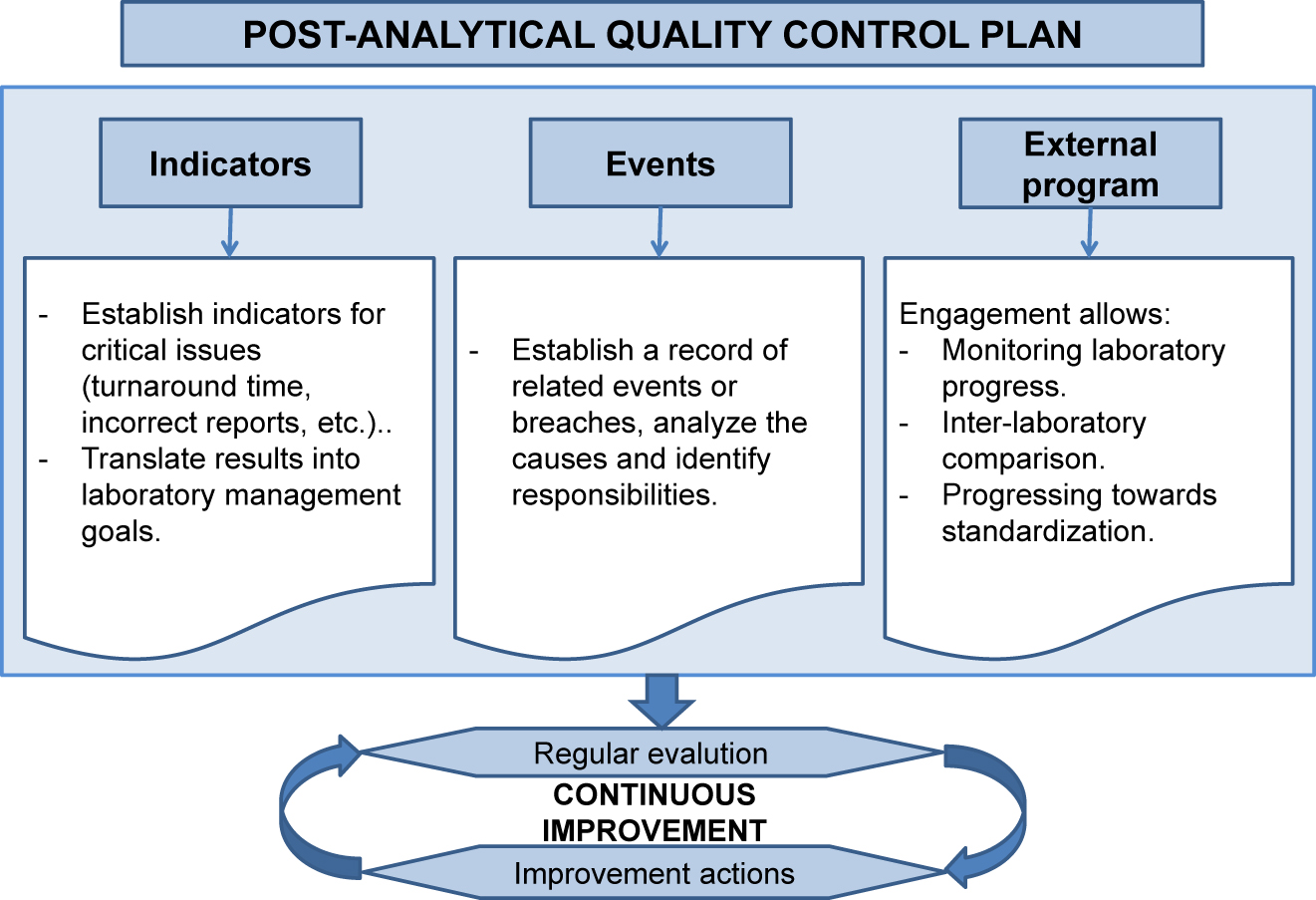
Quality assurance and continuous improvement
As with pre-analytical and analytical procedures, post-analytical procedures must be evaluated and audited to ensure compliance with standards. Auditing is also intended to verify whether the process satisfies user’s needs and requirements. Thus, efforts are necessary to improve the effectiveness of the post-analytical process.
Evaluation of the post-analytical process must include the activities carried out both in the laboratory (post-analytical phase) and out of the laboratory (post-post-analytical phase). A range of studies have demonstrated that most errors occur in the post-post-analytical phase due to the variety of services and number of external professionals involved.[7]
The incidence of errors in the post-analytical process varies significantly, from 18%[8] to 47%[9] of total errors. The most frequent errors include misinterpretation of test results by the laboratory, delayed delivery of reports, loss of reports, and failure to report specimen-related events to the requesting physician. Post-analytical errors may lead to incorrect clinical decisions based on a misinterpretation of test results. Poor decision-making may affect the clinical course, prognosis, and outcome of the patient. These are traditionally called post-post-analytical phase/process errors.[8][9][10] These processes can be improved by enhancing interaction between the professionals involved, where communication and training play a crucial role.[11] Another potential source of errors that is expected to increase in the future is the inability to check test results in the electronic health record (EHR) of the patient due to technical issues.
The laboratory is required to design a quality control plan to verify whether post-analytical activities meet the established standards. This control is primarily based on strategies aimed at detecting errors and establishing quality indicators (see Figure 2).
|
Quality indicators of post-analytical processes allow for the objective evaluation of the service delivered to ensure the quality of this process based on compliance with quality standards. For a proper evaluation of results, it is essential that communication between laboratory staff and ordering physicians is regular, fluid, and based on a standard protocol. Indicators of the post-analytical process include reference intervals, cut-off points, action points, graphic representation, self-validation, interpretative comments, reflex tests (i.e., tests automatically performed on the basis of an algorithm), or reflective tests (i.e., tests added by a professional considering the clinical context)[12][13], the clinical information required for the correct interpretation of results, reporting of critical values, and effective release of laboratory test results through the laboratory information system (LIS).[14] According to numerous users, the most important indicator of laboratory performance is the time period between a test request and delivery of results (turnaround time), which is especially relevant for patients seen in or admitted to emergency care.
A model of quality indicators was presented at the Consensus Conference held in Padua in 2013, which assigns a priority score to each indicator to help laboratories implement effective interventions to improve performance. A criterion was proposed for the establishment of quality standards to assess laboratory performance.[14] In the 2016 Padua Conference, a review was performed of the results obtained since 2014 to identify the indicators and quality standards that should be established to comply with ISO 15189:2012 requirements through continuous monitoring of critical activities to minimize risks. The established indicators evaluate all post-analytical stages, from result validation to the effective, timely result release. Indicators are expressed as a percentage of errors in each laboratory activity. The way each activity is expressed is essential (number of requests, patients, samples, among others), since it will allow inter-laboratory comparison (benchmarking) or comparison against recommendations of scientific societies and entities. The indicators included in the Padua consensus statement are detailed in Table 1.
| Table 1. Indicators included in the Padua Consensus Statement on the post-analytical process, based upon indicators from the International Federation of Clinical Chemistry and Laboratory Medicine Working Group[15] | ||
| Activity | Description | Calculation formula |
|---|---|---|
| Turnaround time | Number of reports issued not complying with the agreed timeframe with respect to the total number of reports | Number of out-of-time reports/total number of reports in a year × 100 (%) |
| Turnaround time | Turnaround time for different analytes (potassium, INR, WBC, troponin I or T) from request receipt to result report | Day and time of issue – day and time of entry (day, time (h/min)); Note: “… for non-emergency analysis of serum potassium concentrations.” |
| Corrected laboratory reports | Percentage of reports corrected by the laboratory after delivery with respect to the total number of reports | Number of corrected reports in a year/total number of reports in a year × 100 (%) |
| Critical result notification | Critical results reported out of time with respect to the total number of reported results | Number of critical results reported out of time in a year/Total number of critical results in a year × 100 (%); Note: “… for all tests with indication of emergency report” and “… for non-emergency analysis of serum potassium concentrations, etc.” |
| Critical result notification | Mean time to critical result notification | Mean (time of result notification – time of result release to the ordering physician (min)); Note: “… for all tests with indication of emergency report” and “… for non-emergency analysis of serum potassium concentrations, etc.” |
References
- ↑ López Yeste, Ma Liboria; Izquierdo Álvarez, Silvia; Pons Mas, Antonia R.; Álvarez Domínguez, Luisa; Blanco Font, Aurora; Marqués García, Fernando; Bernabeu Andreu, Francisco A.; Rodríguez, Ma Patrocinio Chueca et al. (10 March 2021). "Gestión del proceso posanalítico en los laboratorios clínicos según los requisitos de la norma ISO 15189:2012. Consideraciones sobre la revisión, notificación y comunicación de los resultados" (in en). Advances in Laboratory Medicine / Avances en Medicina de Laboratorio 2 (1): 61–70. doi:10.1515/almed-2020-0027. ISSN 2628-491X. https://www.degruyter.com/document/doi/10.1515/almed-2020-0027/html.
- ↑ "UNE-EN ISO 15189:2013". Tienda AENOR. AENOR. 12 June 2013. https://tienda.aenor.com/norma-une-en-iso-15189-2013-n0051322.
- ↑ "CGA-ENAC-LCL Rev. 3 Criterios generales de acreditación de Laboratorios Clínicos" (PDF). ENAC. September 2018. https://www.enac.es/documents/7020/b569e184-a2aa-4dcd-88a5-1d1ceb9033db.
- ↑ Beastall, Graham H. (1 January 2013). "Adding value to laboratory medicine: a professional responsibility" (in en). Clinical Chemistry and Laboratory Medicine (CCLM) 51 (1): 221–227. doi:10.1515/cclm-2012-0630. ISSN 1437-4331. https://www.degruyter.com/document/doi/10.1515/cclm-2012-0630/html.
- ↑ "CEA-ENAC-01 Criterios para la utilización de la marca ENAC o referencia a la condición de acreditado" (PDF). ENAC. April 2020. https://www.enac.es/documents/7020/88f9773a-6214-45ef-9618-3b7efc549699.
- ↑ Alsina, M.J.; Álvarez, V.; Bueno, M. et al. (2006). "Protocolo para el estudio de la estabilidad de las magnitudes biológicas". Química Clínica 25 (2): 86–89. https://www.seqc.es/download/doc/21/2796/759467396/69509/cms/protocolo-para-el-estudio-de-la-estabilidad-de-las-magnitudes-biologicas-2006.pdf/. Retrieved 16 November 2020.
- ↑ Aarsand, Aasne K.; Sandberg, Sverre (1 May 2014). "How to achieve harmonisation of laboratory testing —The complete picture" (in en). Clinica Chimica Acta 432: 8–14. doi:10.1016/j.cca.2013.12.005. https://linkinghub.elsevier.com/retrieve/pii/S0009898113004890.
- ↑ 8.0 8.1 Plebani, Mario; Laposata, Michael; Lundberg, George D. (1 December 2011). "The Brain-to-Brain Loop Concept for Laboratory Testing 40 Years After Its Introduction" (in en). American Journal of Clinical Pathology 136 (6): 829–833. doi:10.1309/AJCPR28HWHSSDNON. ISSN 1943-7722. https://academic.oup.com/ajcp/article/136/6/829/1760426.
- ↑ 9.0 9.1 Ajzner, Éva (20 April 2016). "Adding Value in the Postanalytical Phase". EJIFCC 27 (2): 166–173. ISSN 1650-3414. PMC 4975232. PMID 27683529. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4975232/.
- ↑ Plebani, Mario (1 January 2006). "Errors in clinical laboratories or errors in laboratory medicine?". Clinical Chemistry and Laboratory Medicine (CCLM) 44 (6). doi:10.1515/CCLM.2006.123. ISSN 1434-6621. https://www.degruyter.com/document/doi/10.1515/CCLM.2006.123/html.
- ↑ Plebani, Mario; Panteghini, Mauro (1 May 2014). "Promoting clinical and laboratory interaction by harmonization" (in en). Clinica Chimica Acta 432: 15–21. doi:10.1016/j.cca.2013.09.051. https://linkinghub.elsevier.com/retrieve/pii/S0009898113003999.
- ↑ Verboeket-van de Venne, Wilhelmine P.H.G.; Aakre, Kristin M.; Watine, Joseph; Oosterhuis, Wytze P. (1 July 2012). "Reflective testing: adding value to laboratory testing" (in en). Clinical Chemistry and Laboratory Medicine (CCLM) 50 (7): 1249–1252. doi:10.1515/cclm-2011-0611. ISSN 1437-4331. https://www.degruyter.com/document/doi/10.1515/cclm-2011-0611/html.
- ↑ Srivastava, Rajeev; Bartlett, William A; Kennedy, Ian M; Hiney, Allan; Fletcher, Colin; Murphy, Michael J (1 May 2010). "Reflex and reflective testing: efficiency and effectiveness of adding on laboratory tests" (in en). Annals of Clinical Biochemistry: International Journal of Laboratory Medicine 47 (3): 223–227. doi:10.1258/acb.2010.009282. ISSN 0004-5632. http://journals.sagepub.com/doi/10.1258/acb.2010.009282.
- ↑ 14.0 14.1 Sciacovelli, Laura; Aita, Ada; Padoan, Andrea; Pelloso, Michela; Antonelli, Giorgia; Piva, Elisa; Chiozza, Maria Laura; Plebani, Mario (1 January 2016). "Performance criteria and quality indicators for the post-analytical phase". Clinical Chemistry and Laboratory Medicine (CCLM) 54 (7). doi:10.1515/cclm-2015-0897. ISSN 1437-4331. https://www.degruyter.com/document/doi/10.1515/cclm-2015-0897/html.
- ↑ "Laboratory Errors and Patient Safety" (PDF). International Federation of Clinical Chemistry and Laboratory Medicine Working Group. January 2017. https://www.ifcc.org/media/455725/Quality_Indicators_Key_Processes.pdf. Retrieved 16 November 2020.
Notes
This presentation is faithful to the original, with only a few minor changes to presentation, spelling, and grammar. In some cases important information was missing from the references, and that information was added.