Journal:Evaluating the effectiveness of a new student-centred laboratory training strategy in clinical biochemistry teaching
| Full article title | Evaluating the effectiveness of a new student-centred laboratory training strategy in clinical biochemistry teaching |
|---|---|
| Journal | BMC Medical Education |
| Author(s) | Xu, Guoying; Zhao, Chuanxiang; Yan, Mengdan; Zhang, Xiaoxian; Zhu, Ling; Liu, Jiaxiu; Zhao, Yaping; Zhang, Yuling; Cai, Weili; Xie, Hongxiang; Jiang, Yuzhang; Shao, Qixiang |
| Author affiliation(s) | Jiangsu College of Nursing, Youyang Medical Laboratory Co., Hangzhou Medical College, Nanjing Medical University |
| Primary contact | Email: shao underscore qx at jscn dot edu dot cn |
| Year published | 2023 |
| Volume and issue | 23 |
| Article # | 391 |
| DOI | 10.1186/s12909-023-04272-7 |
| ISSN | 1472-6920 |
| Distribution license | Creative Commons Attribution 4.0 International |
| Website | https://bmcmededuc.biomedcentral.com/articles/10.1186/s12909-023-04272-7 |
| Download | https://bmcmededuc.biomedcentral.com/counter/pdf/10.1186/s12909-023-04272-7.pdf (PDF) |
Abstract
Background: The error-proneness in the pre-analytical and post-analytical stages is higher than that in the analytical stage of the total laboratory testing process. However, pre-analytical and post-analytical quality management has not received enough attention in medical laboratory education and tests in clinical biochemistry courses.
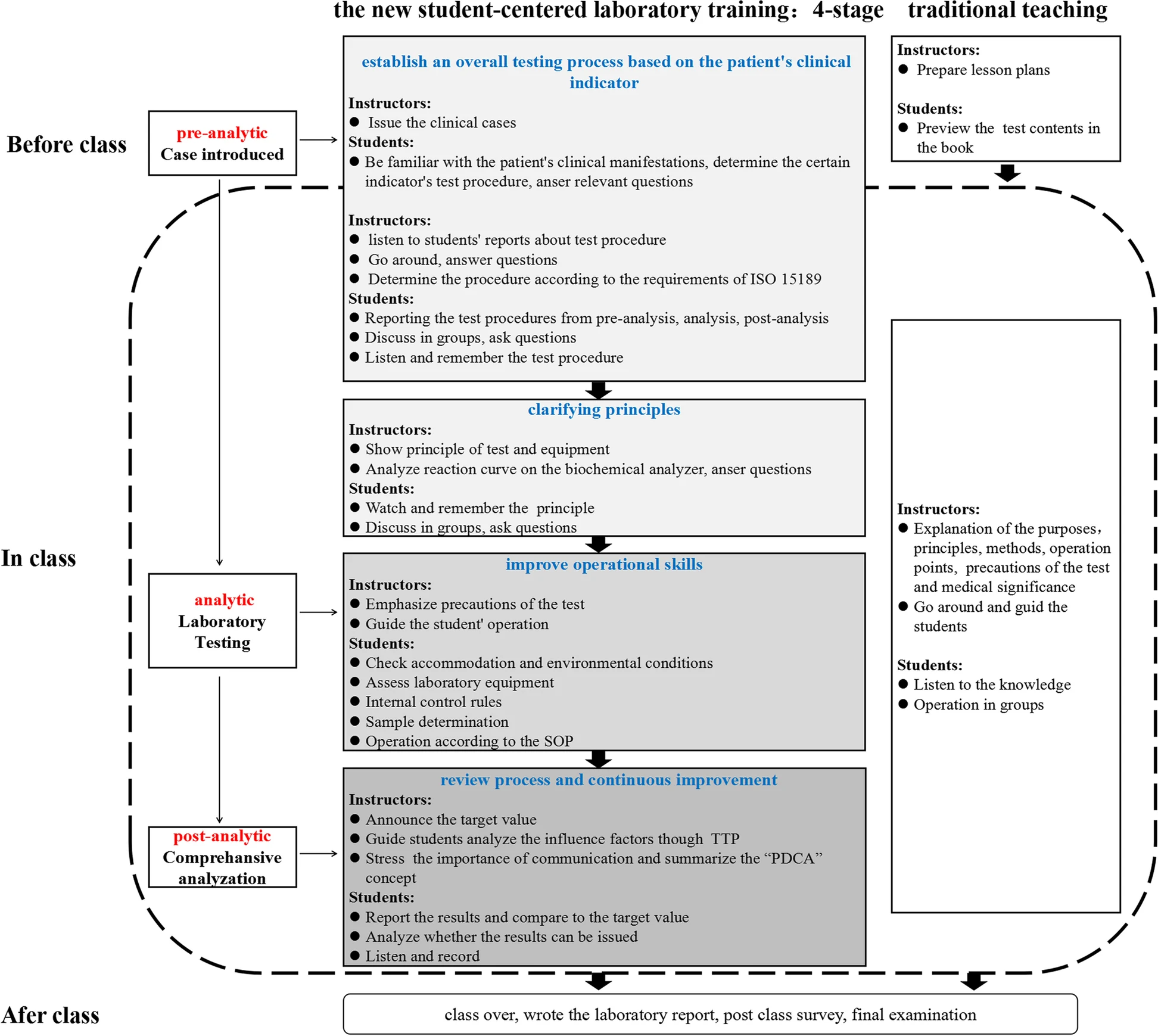
Methods/approach: Clinical biochemistry teaching programs aim to improve students’ awareness of and ability to use quality management practices according to the International Organization for Standardization's ISO 15189 requirements. We designed a student-centered laboratory training program according to case-based learning that included four stages: establish an overall testing process based on the patient’s clinical indicators, clarify principles, improve operational skills, and review processes and continuous improvement opportunities. The program was implemented in our college during the winter semesters of 2019 and 2020. A total of 185 undergraduate students majoring in medical laboratory science participated in the program as a test group, and the other 172 students were set up as the control group and adopted the conventional method. The participants were asked to finish an online survey to evaluate the class at the end.
Results/outcomes: The test group had significantly better examination scores not only in experimental operational skills (89.27 ± 7.16 vs. 77.51 ± 4.72, p < 0.05 in 2019 grade, 90.31 ± 5.35 vs. 72.87 ± 8.41 in 2020 grade) but also in total examination (83.47 ± 6.16 vs. 68.90 ± 5.86 in 2019 grade, 82.42 ± 5.72 vs. 69.55 ± 7.54 in 2020 grade) than the control group. The results of the questionnaire survey revealed that the students in the test group better achieved classroom goals than those in the control group (all p < 0.05).
Conclusions: The new student-centered laboratory training program based on case-based learning in clinical biochemistry is an effective and acceptable strategy compared with the conventional training program.
Keywords: case-based learning, clinical biochemistry, laboratory training, quality management, student-centered
Introduction
Clinical biochemistry is a pivotal division of the modern medical laboratory. According to the International Federation of Clinical Chemistry (IFCC), clinical chemistry is responsible for applying chemical, molecular, and cellular strategies and techniques to better understand and assess human health and disease processes. It ultimately affects the process of treatment as well as the quality of medical outcomes.[1] It has been reported that the results of laboratory tests influence 70 percent of medical diagnoses, guide approximately 70 percent of clinical decisions, and facilitate the provision of optimal patient care.[2][3]
Practical training plays a crucial role in clinical biochemistry curriculum. The goal of the course is to enable students to remember the test procedure and understand the underlying principles and medical significance, especially to ensure the accuracy of the test results. However, in traditional teaching, emphasis on quality control (QC) during the analytical process has received more attention, while neglecting elements of QC during the pre-analytical and post-analytical processes in the experimental courses of clinical biochemistry teaching. In fact, the error-proneness in the analytical process is lower than that in pre- and post-analytical processes of the total testing process (TTP).[4] Moreover, awareness of and ability to use quality management practices are much more important for students. The International Organization for Standardization's (ISO's) ISO 15189 Medical laboratories — Requirements for quality and competence was first published by the ISO's Clinical laboratory testing and in vitro diagnostic test systems technical committee (ISO/TC 212) in 2003. After several revisions, it has become an important international gold standard in medical laboratory proficiency, cultivating strong elements of laboratory quality management while addressing the processes and procedures that should be used throughout the TTP.[5][6] As such, there is strong value in acclimating students to the concepts of quality management by applying the ISO 15189 standard to clinical biochemistry classwork.
Traditional training models such as lecture-based learning (LBL) have several features, including a teacher-centered tiered process, a focus on knowledge acquisition, and a final summative assessment at the end of courses. This is indeed the most cost-effective way to carry out theoretical education.[7] As such, several teaching modes are obviously superior to traditional teaching in the course of clinical biochemistry, such as traditional teaching combined with group discussion, peer debriefing approaches, and team learning.[8][9][10] However, small groups and case-based learning (CBL) are likely to dominate medical education. CBL is a learner-centered special type of problem-based learning (PBL) that guides students’ learning and exploration through cases. It has been elucidated that CBL can improve the performance and clinical skills of medical students[11]; help convey an understanding of key concepts[12]; improve clinical practice, problem-solving, case analysis, and the link between theory and practice[13][14][15]; and motivate students to learn more deeply[16], with better student satisfaction.[17] It is hypothesized that students who participate in CBL gain deeper and longer lasting knowledge than those who do not.[18] Compared with traditional methods, the application of practical knowledge (Objective Structure Clinic Examination [OSCE] scores) through CBL is significantly improved.[19]
A limitation of this approach is that multiple faculty facilitators may be needed. However, during the COVID-19 pandemic, virtual teaching workshops emerged as an easy and straightforward way to implant a more interactive format into virtual case teaching for health professions.[20] That being said, there is yet to appear a proper teaching model that focuses on improving the entire quality management process dictated by ISO 15189 in clinical biochemistry courses.
Here, we designed a new student-centered training program based on CBL in the experimental teaching of a clinical biochemistry course, with the goal of improving the awareness of and ability to use quality management practices by students majoring in medical laboratory science.
Methods
Participants
A total of 357 undergraduate students majoring in medical laboratory science in 2019 and 2020 were randomly divided into two groups: a test group and a control group. Students participated in the program each semester. There were 92 recruited into the testing group in 2019 and 93 recruited into 2020 according to individual will. The number of male and female students was kept similar to exclude the influencing factors of gender on CBL.[13] The remaining students (87 in 2019, 85 in 2020) participated in the traditional program as a control group. Teachers with at least one year of CBL teaching experience were designated as the teachers of the test group, which enrolled 10 to 12 students per training classroom. All study participants completed basic medical courses related to the testing profession and had a certain ability to comprehensively analyze medical knowledge. Students from both groups were taught by the same teachers using the same syllabus and teaching materials. In this study, no significant differences were found between the study participants, such as the theoretical score of biochemistry and clinical disease synopsis course. The control group was given appropriate supplementary training after the examination to prevent perceived unfairness in their education experience. All the programs were approved by the education committee of our college.
Teaching strategies
A total of nine experiments were assigned. The primary subject was on biosafety and the use of biochemical instruments commonly used in clinical practice. The themes of the remaining eight classes involved specific experiments on clinical indicators of diabetes mellitus, liver cirrhosis, nephrotic syndrome, coronary atherosclerotic cardiopathy, pancreatitis, electrolyte disturbance, multiple myeloma, and hyperthyroidism. At the end of program, the lab examination was performed. Each experiment was conducted in three consecutive classes of 45 minutes. A similar learning environment was maintained for both groups, i.e., lab classrooms, lecture times, assessment methods.
Test group
The laboratory training adopted a new student-centered training program that was divided into four stages. First, students had access to the case (with the questions) at least two to four days before the class and were asked to answer several basic questions individually about the case before the class, e.g., what the diagnosis is based on, what the detection indicators are, and what the the indicators of a certain inspection procedures for pre-analysis, analysis, and post-analysis are. The answers of each minor group were then shared in the class, and the students tried to reach a consensus among the groups, with the teachers’ facilitation. This stage took approximately 30 minutes. Second, it took 30 minutes to learn principles, which was mainly an explanation of the current commonly used methods and principles. Third, it took 45 minutes to improve their lab skills, including the evaluation of lab conditions, assessment of equipment conditions, use of internal control, and sample processing according to the standard operating procedure (SOP). Fourth, results were analyzed by combining the ISO 15189 requirements with the teaching contents to improve the operations in 30 minutes. The main concern was the review and reporting of results. When abnormal or suspicious results occurred, the students were able to identify them. The teachers facilitated the entire process. If the results were not judged correctly, the teacher asked students to re-check the result until they met the re-inspection requirements, and the students analyzed whether the results could be issued. After that, the students were asked to conduct a quiz and an after-class survey.
Control group
The knowledge and theoretical outline of the clinical biochemistry course in the lectures was the same as that of the test group. Experimental teaching was implemented in a teacher-centered way. The teacher explained the principles, operation points, and medical significance, and then the students performed the experiment. A schematic diagram of the teaching mode between the two groups is shown in Figure 1.
|
Here is an example. Students became familiar with the clinical manifestations of a patient with recurrent systemic edema (finally diagnosed as nephrotic syndrome) two weeks before the class on that same topic. When the nephrotic syndrome was diagnosed, urinalysis, blood counts and coagulation panel, renal function and electrolytes, liver panel, and glucose tests were required. Students were asked to report why and how the test procedure for “creatine and urea” in renal function was determined. Finally, students were then asked to discuss the examination process and medical significance, and analyze various factors that may affect the test result, including pre-pre-analysis (i.e., test selection, test ordering, patient/specimen identification), pre-analysis (i.e., specimen collection, transportation, specimen processing, specimen preparation), analytic, post-analysis (i.e., report review, result reporting), and post-post-analysis (i.e., result interpretation) in accordance with the requirements of ISO 15189.[21] Then students made an operation plan according to the inspection process of the project, and the teachers evaluated and determined the testing procedure.
Outcome evaluation
Assessment for laboratory operation
To evaluate students’ students’ awareness of and ability to use quality management practices in TTP and other laboratory processes, evaluation indicators were designed as shown in Table 1.
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Assessment of students’ course scores
The total course scores included four components: classroom performance, experimental evaluation, mid-term examination, and final examination (Table 2). Classroom performance includes attendance, attitude, completeness of assignment, and experiment report. The content of the experiment report includes four parts: how to determine the test procedure, test principle, precautions of the procedure, and results interpretation and analysis. The experimental evaluation was carried out in the last class. The eight items were numbered, and the students drew lots to determine which items to evaluate. The mid-term and final exams had terminology, short answers, and single-choice questions: 10 fill-in-the-blank (one point per question); five terminology (two points per question); four short-answer questions, including one case analysis (five points per question); and 60 single-choice (one point per question). Standard answers to all questions were defined by the instructor before the students’ answers were graded.
| ||||||||||||||||||
Questionnaire survey
Curriculum evaluation is critical to continuous assurance of teaching quality.[22] To assess the effectiveness and acceptability of implementing the four-stage experimental training program based on the ISO 15189 standard, in addition to the typical course evaluations, the students were asked to complete a survey about the course after finishing the course. An anonymous 10-question survey was created to develop a baseline of student achievement of goals in the class and the impact of teaching mode on learning (Table 3). The questions presented in the results section were discussed by all supervisors involved in this study to ensure their quality. Most of the survey questions were in Likert scale format, giving a statement on a scroll bar that the students could choose from “Strongly Disagree” to “Strongly Agree” on a scale of 1-5.
| ||||||||||||||||||||||||||
Statistical analysis
Means and standard deviations were calculated, and the differences were analyzed using an independent samples t test. A p value < 0.05 was considered to be statistically significant. Data are presented as the means ± SDs.
Results
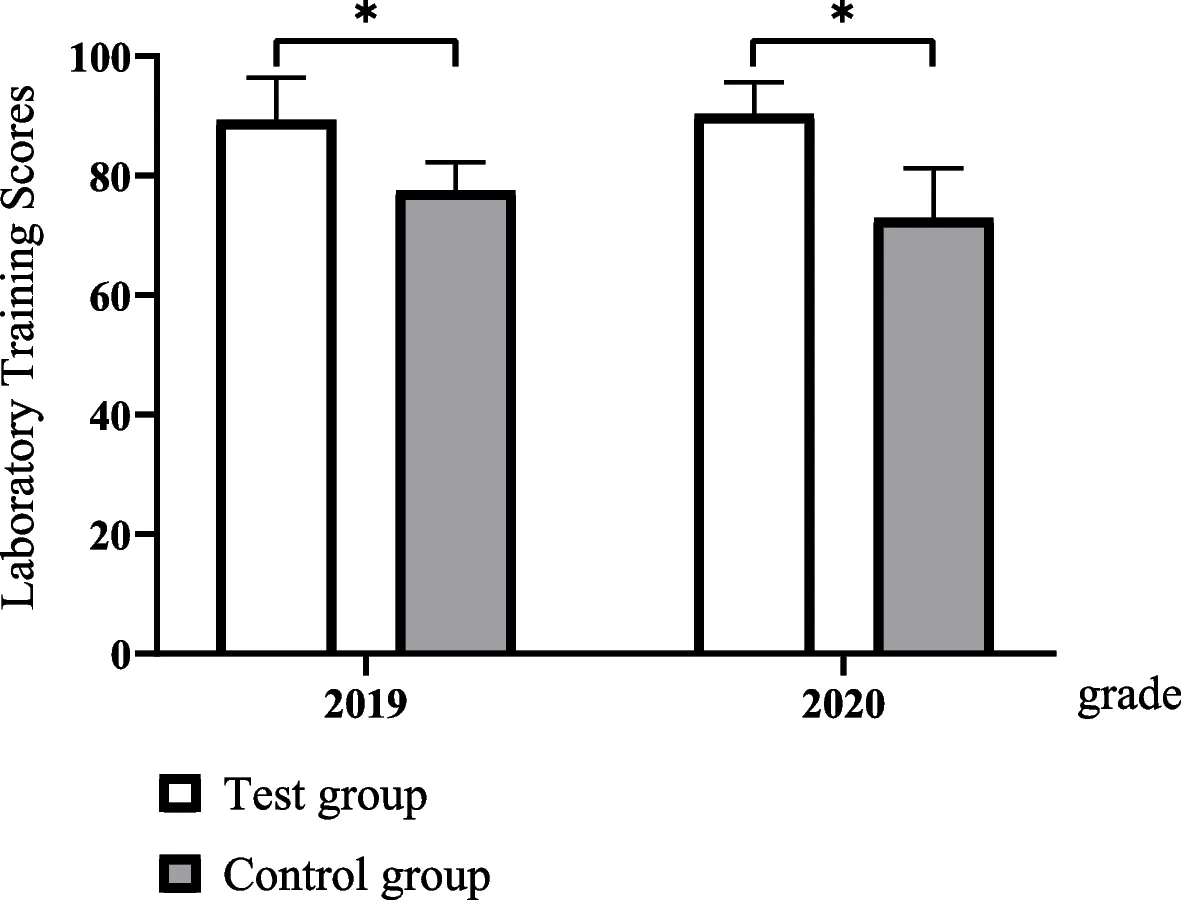
Comparison of laboratory training scores
A total of 357 students participated in this program, and 185 students (52%) attended a four-stage training program. A total of 314 students completed the post-class survey (88% response rate).
The experimental operation scores in four-stage training program classes were significantly higher than those of the traditional program classes of both grades (Fig. 2).
|
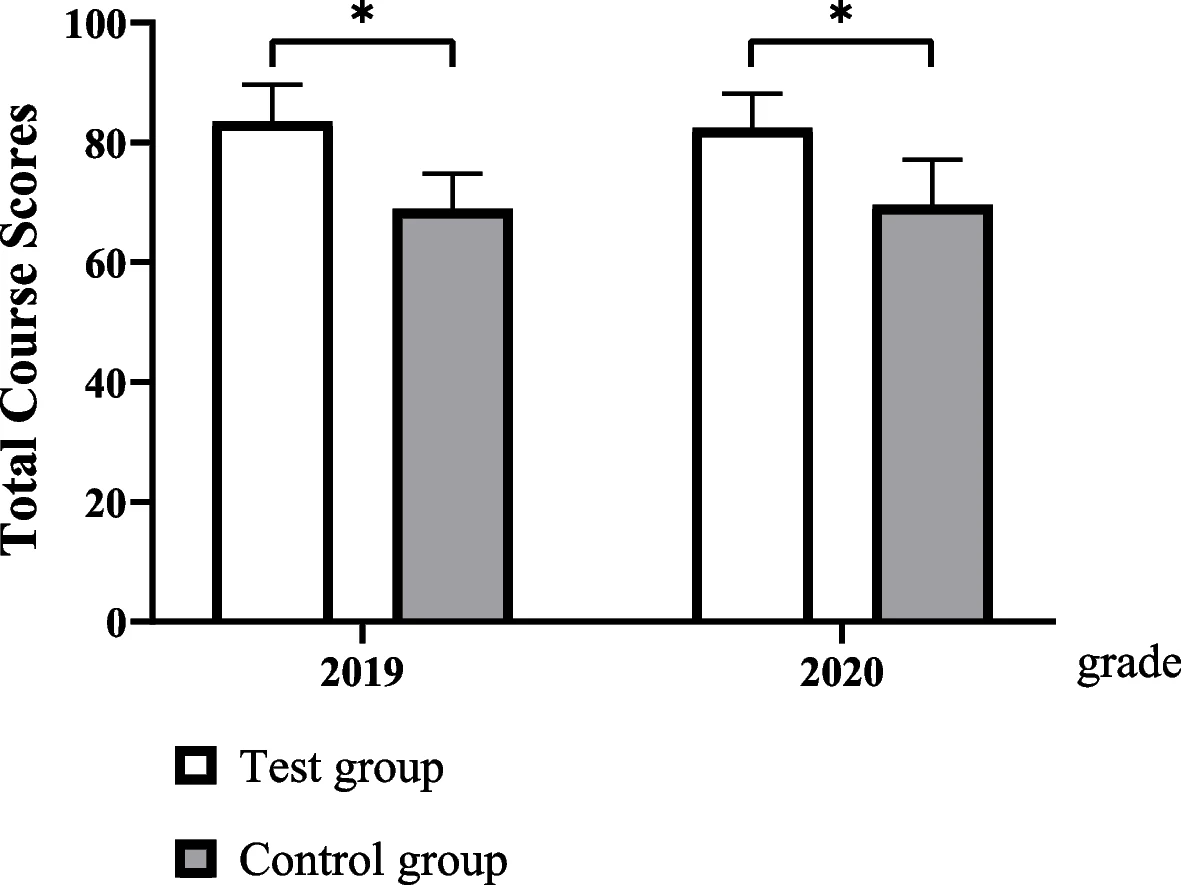
Comparison of total course scores
The students’ scores for this course in the test groups were significantly higher than those in the control groups in 2019 and 2020 (Fig. 3).
|
Survey results
The accumulative score on the survey questions on learning for the students in the test group was higher than that for the students in the control group either about objectives or the impact of teaching mode on learning (Table 4). Students in the testing group agreed that they remembered the testing procedure, understood the testing principle and the medical significance, understood the connotation of ISO 15189 requirements, and agreed that quality management is more important than QC. Fewer students in the control group agreed. More students were interested and satisfied with this new student-centered teaching mode. Meanwhile, more students would like the teaching model to be used in other courses.
| ||||||||||||||||||||||
Discussion
Clinical biochemistry belongs to the field of medical technology and involves various techniques and methods for analyzing the chemical components of body fluid samples.[23] To do well in the clinical biochemistry course, students will undergo rigorous clinical laboratory practical training and gain valuable practical experience in sample handling and instrumentation. Ensuring the accuracy of test results and understanding the medical significance of laboratory tests are important for students who major in medical laboratories. There are many obstacles to teaching clinical chemistry and laboratory medicine, such as the lack of interactive or hands-on teaching models.[24] In this study, we designed a new student-centered training program with four stages based on CBL considering TTP, including pre-analytical, analytical, and post-analytical stages. The participating teachers were asked to provide clinical cases related to clinical biochemistry, design questions according to the experimental objectives, and upload to the DingTalk group before class. Reaction curves on an automated biochemical analyzer were also provided. CBL requires students to prepare well in advance, which may be considered an additional burden if they are not yet familiar with the subject of the course.[25][26] The authors suggest that CBL should be actively adopted for courses that are delivered in the final stage of the program. The quality of students’ previews directly affects the learning effect of each stage. In particular, the determination of the process of the first stage of the inspection program process and the analysis of errors in the final stage from pre-analysis to post-analysis.
Our new student-centered training strategy has a positive effect on both the achievement of class goals and the impact of teaching mode on learning. It has several advantages over traditional teaching methods. First, it helps students combine the theory with complicated clinical situations. With cases as a bridge, to explore as a driving force, students can integrate their knowledge and adapt to clinical practice. Second, under the new training evaluation system, students pay more attention to the management of the entire testing process rather than on the QC of the analysis, as the error rate of the analysis is lower than that of the pre-analysis and post-analysis of the TTP. Third, by analyzing the experimental results and unconsciously recording the test process, ISO 15189 concepts of continuous improvement were implanted, thereby putting the concept of plan–do–check–act (PDCA) into practice, developing recording habits, and improving communication skills.
While the program has already produced very positive results, there are many improvements and additions that could be made. The first would be to check students’ familiarity with the case before the class. Otherwise, the first stage of the study time could be extended. In addition, multiple discipline inspection items, such as immunology, microbiology, and clinical examination, should be considered based on the symptoms of each patient. Different assignments of students may affect the course sores between the two groups.
Conclusion
In summary, our experience suggests that this new student-centered experimental teaching strategy based on CBL is more effective and acceptable than the conventional experimental teaching mode in the clinical biochemistry course.
Abbreviations, acronyms, and initialisms
- CBL: case-based learning
- IFCC: International Federation of Clinical Chemistry
- ISO: International Organization for Standardization
- LBL: lecture-based learning
- OSCE: Objective Structure Clinic Examination
- PBL: problem-based learning
- PDCA: plan–do–check–act
- QC: quality control
- SOP: standard operating procedure
- TTP: total testing process
Acknowledgements
The authors thank all the students who participated in the study.
Author contributions
Guoying Xu, Chuanxiang Zhao, Mengdan Yan, Xiaoxian Zhang, Ling Zhu, Jiaxiu Liu, and Qixiang Shao conceived the training program. Yuzhang Jiang, Yaping Zhao and Hongxiang Xie put forward many suggestions during the implementation of the program. Guoying Xu, Yuling Zhang and Qixiang Shao performed the analysis and interpreted the data. Guoying Xu wrote the original graft. Weili Cai and Qixiang Shao helped organize and revise the manuscript. All authors read and approved the final manuscript. Guoying Xu and Xiaoxian Zhang are the funding recipients. All authors contributed to the article and approved the submitted version.
Ethics approval and consent to participate
This study was performed in accordance with the Declaration of Helsinki. It was approved by the Ethics Committee of Huai’an First People’s Hospital. Informed consent was obtained from all subjects.
Funding
This work was supported by the fifth issue of Jiangsu Province Vocational Education Teaching Reform Research Project (ZYB545), Program of China Vocational Education Society (ZJS2022YB214), and Program of the Key Laboratory Construction of Innovation Service Capacity Construction Plan of Huai ‘an Science and Technology Bureau (HAP202004).
Availability of data and materials
The datasets used and/or analyzed in this study are available from the corresponding authors on reasonable request.
Competing interests
The authors declare that they have no competing interests.
References
- ↑ Durner, Jürgen (29 December 2009). "Clinical Chemistry: Challenges for Analytical Chemistry and the Nanosciences from Medicine" (in en). Angewandte Chemie International Edition 49 (6): 1026–1051. doi:10.1002/anie.200903363. https://onlinelibrary.wiley.com/doi/10.1002/anie.200903363.
- ↑ Silverstein, M.D. (3 April 2003). "An Approach to Medical Errors and Patient Safety in Laboratory Services: A White Paper Prepared for the Quality Institute Meeting "Making the Laboratory a Partner in Patient Safety," Atlanta, April 2003" (PDF). Centers for Disease Control and Prevention. https://www.researchgate.net/profile/Marc-Silverstein/publication/237739475_An_Approach_to_Medical_Errors_and_Patient_Safety_in_Laboratory_Services_A_White_Paper_Prepared_for_the_Quality_Institute_Meeting_Making_the_Laboratory_a_Partner_in_Patient_Safety_Atlanta_April_2003_Di/links/0deec53a04e183b191000000/An-Approach-to-Medical-Errors-and-Patient-Safety-in-Laboratory-Services-A-White-Paper-Prepared-for-the-Quality-Institute-Meeting-Making-the-Laboratory-a-Partner-in-Patient-Safety-Atlanta-April-2003-D.pdf.
- ↑ Guzel, Omer; Guner, Ebru Ilhan (1 March 2009). "ISO 15189 Accreditation: Requirements for quality and competence of medical laboratories, experience of a laboratory I" (in en). Clinical Biochemistry 42 (4-5): 274–278. doi:10.1016/j.clinbiochem.2008.09.011. https://linkinghub.elsevier.com/retrieve/pii/S0009912008003998.
- ↑ Lippi, Giuseppe; Mattiuzzi, Camilla; Bovo, Chiara (5 February 2018). "Are we getting better at the preanalytical phase or just better at measuring it?". Journal of Laboratory and Precision Medicine 3: 11–11. doi:10.21037/jlpm.2018.01.03. http://jlpm.amegroups.com/article/view/3992/4747.
- ↑ International Organization for Standardization (November 2012). "ISO 15189:2012 Medical laboratories — Requirements for quality and competence". https://www.iso.org/standard/56115.html.
- ↑ Aslan, Diler (5 December 2018). "Which Skills are Needed and How They Should be Gained by Laboratory Medicine Professionals for Successful ISO 15189 Accreditation". EJIFCC 29 (4): 264–273. ISSN 1650-3414. PMC 6295584. PMID 30574036. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6295584/.
- ↑ Oderinu, Olabisi H.; Adegbulugbe, Ilemobade C.; Orenuga, Omolola. O.; Butali, Azeez (1 May 2020). "Comparison of students' perception of problem‐based learning and traditional teaching method in a Nigerian dental school" (in en). European Journal of Dental Education 24 (2): 207–212. doi:10.1111/eje.12486. ISSN 1396-5883. https://onlinelibrary.wiley.com/doi/10.1111/eje.12486.
- ↑ Vadakedath, Sabitha; Kandi, Venkataramana (16 August 2019). "Modified Conventional Teaching: An Assessment of Clinical Biochemistry Learning Process Among Medical Undergraduate Students Using the Traditional Teaching in Combination with Group Discussion" (in en). Cureus. doi:10.7759/cureus.5396. ISSN 2168-8184. PMC PMC6793614. PMID 31620321. https://www.cureus.com/articles/22339-modified-conventional-teaching-an-assessment-of-clinical-biochemistry-learning-process-among-medical-undergraduate-students-using-the-traditional-teaching-in-combination-with-group-discussion.
- ↑ Fatima, Syeda; Liaquat, Afrose; Mansoor, Sumreena; Rauf, Ayesh; Fatima, Syeda (2020). "Clinical biochemistry teaching: use of peer debriefing by Pendleton's rule as an instructional tool". Journal of the Pakistan Medical Association (0): 1. doi:10.5455/JPMA.17645. ISSN 0030-9982. https://www.ejmanager.com/fulltextpdf.php?mno=17645.
- ↑ Alamoudi, Aliaa Amr; Al Shawwa, Lana Adey; Gad, Hoda; Tekian, Ara (1 July 2021). "Team‐based learning versus traditional didactic lectures in teaching clinical biochemistry at King Abdulaziz University; learning outcomes and student satisfaction" (in en). Biochemistry and Molecular Biology Education 49 (4): 546–559. doi:10.1002/bmb.21501. ISSN 1470-8175. https://iubmb.onlinelibrary.wiley.com/doi/10.1002/bmb.21501.
- ↑ Zhao, Wanjun; He, Linye; Deng, Wenyi; Zhu, Jingqiang; Su, Anping; Zhang, Yong (1 December 2020). "The effectiveness of the combined problem-based learning (PBL) and case-based learning (CBL) teaching method in the clinical practical teaching of thyroid disease" (in en). BMC Medical Education 20 (1): 381. doi:10.1186/s12909-020-02306-y. ISSN 1472-6920. PMC PMC7583209. PMID 33092583. https://bmcmededuc.biomedcentral.com/articles/10.1186/s12909-020-02306-y.
- ↑ Novack, Jeffrey P. (27 May 2020). "Designing Cases for Case-Based Immunology Teaching in Large Medical School Classes". Frontiers in Immunology 11: 995. doi:10.3389/fimmu.2020.00995. ISSN 1664-3224. PMC PMC7267000. PMID 32536919. https://www.frontiersin.org/article/10.3389/fimmu.2020.00995/full.
- ↑ 13.0 13.1 Williams, B (1 August 2005). "Case based learning--a review of the literature: is there scope for this educational paradigm in prehospital education?" (in en). Emergency Medicine Journal 22 (8): 577–581. doi:10.1136/emj.2004.022707. ISSN 1472-0205. PMC PMC1726887. PMID 16046764. https://emj.bmj.com/lookup/doi/10.1136/emj.2004.022707.
- ↑ Nair, Sandhya Pillai (2013). "Case Based Learning: A Method for Better Understanding of Biochemistry in Medical Students". JOURNAL OF CLINICAL AND DIAGNOSTIC RESEARCH. doi:10.7860/JCDR/2013/5795.3212. PMC PMC3782900. PMID 24086843. http://www.jcdr.net/article_fulltext.asp?issn=0973-709x&year=2013&volume=7&issue=8&page=1576&issn=0973-709x&id=3212.
- ↑ Cen, X.-Y.; Hua, Y.; Niu, S.; Yu, T. (1 April 2021). "Application of case-based learning in medical student education: a meta-analysis". European Review for Medical and Pharmacological Sciences 25 (8): 3173–3181. doi:10.26355/eurrev_202104_25726. ISSN 1128-3602. https://doi.org/10.26355/eurrev_202104_25726.
- ↑ McLean, Susan F. (1 January 2016). "Case-Based Learning and its Application in Medical and Health-Care Fields: A Review of Worldwide Literature" (in en). Journal of Medical Education and Curricular Development 3: JMECD.S20377. doi:10.4137/JMECD.S20377. ISSN 2382-1205. PMC PMC5736264. PMID 29349306. http://journals.sagepub.com/doi/10.4137/JMECD.S20377.
- ↑ Krupat, Edward; Richards, Jeremy B.; Sullivan, Amy M.; Fleenor, Thomas J.; Schwartzstein, Richard M. (1 May 2016). "Assessing the Effectiveness of Case-Based Collaborative Learning via Randomized Controlled Trial" (in en). Academic Medicine 91 (5): 723–729. doi:10.1097/ACM.0000000000001004. ISSN 1040-2446. https://journals.lww.com/00001888-201605000-00035.
- ↑ Chonkar, Sonali Prashant; Ha, Tam Cam; Chu, Sarah Shan Hang; Ng, Ada Xinhui; Lim, Melissa Li Shan; Ee, Tat Xin; Ng, Mor Jack; Tan, Kok Hian (1 December 2018). "The predominant learning approaches of medical students" (in en). BMC Medical Education 18 (1): 17. doi:10.1186/s12909-018-1122-5. ISSN 1472-6920. PMC PMC5774125. PMID 29347934. https://bmcmededuc.biomedcentral.com/articles/10.1186/s12909-018-1122-5.
- ↑ Turk, Bela; Ertl, Sebastian; Wong, Guoruey; Wadowski, Patricia P.; Löffler-Stastka, Henriette (1 December 2019). "Does case-based blended-learning expedite the transfer of declarative knowledge to procedural knowledge in practice?" (in en). BMC Medical Education 19 (1): 447. doi:10.1186/s12909-019-1884-4. ISSN 1472-6920. PMC PMC6889574. PMID 31796049. https://bmcmededuc.biomedcentral.com/articles/10.1186/s12909-019-1884-4.
- ↑ Spicer, Jennifer O.; Nguyen, Trong Tien; Arnold, Margaret W.; Anderson, Tiffany; Khalife, Roy (17 March 2021). "A Faculty Development Workshop for Planning and Implementing Interactive Virtual Case-Based Teaching" (in en). MedEdPORTAL: 11126. doi:10.15766/mep_2374-8265.11126. ISSN 2374-8265. PMC PMC7970636. PMID 33768155. http://www.mededportal.org/doi/10.15766/mep_2374-8265.11126.
- ↑ Stroobants, A.K; Goldschmidt, H.M.J; Plebani, M (1 July 2003). "Error budget calculations in laboratory medicine: linking the concepts of biological variation and allowable medical errors" (in en). Clinica Chimica Acta 333 (2): 169–176. doi:10.1016/S0009-8981(03)00181-5. https://linkinghub.elsevier.com/retrieve/pii/S0009898103001815.
- ↑ Galukande, M; Katamba, A; Kiguli, S; Kiguli-Malwadde, E; Kijjambu, S; Sewankambo, N (12 March 2015). "Problem based learning: tutors’ views 5 years after implementation at a sub-Saharan University". African Health Sciences 15 (1): 261. doi:10.4314/ahs.v15i1.34. ISSN 1680-6905. PMC PMC4370133. PMID 25834557. http://www.ajol.info/index.php/ahs/article/view/114180.
- ↑ Yao, C.; Li, R.; Fu, W. (2015). "Exploration of the course construction of clinical biochemistry under the new medical model". Zhonghua yixue jiaoyu tansuo zazhi [Chinese Journal of Medical Education Research] 14: 757–60.
- ↑ Wiencek, Joesph R; Chambliss, Allison B; Bertholf, Roger L; Cotten, Steven W; Ellervik, Christina; Kreuter, Justin D; Mirza, Kamran M; Shajani-Yi, Zahra (18 May 2022). "A Paradigm Shift: Engagement of Clinical Chemistry and Laboratory Medicine Trainees by Innovative Teaching Methods" (in en). Clinical Chemistry 68 (5): 619–626. doi:10.1093/clinchem/hvac036. ISSN 0009-9147. https://academic.oup.com/clinchem/article/68/5/619/6548427.
- ↑ Sait, Mohammed Salik; Siddiqui, Zohaib; Ashraf, Yasir (2 May 2017). "Advances in medical education and practice: student perceptions of the flipped classroom" (in English). Advances in Medical Education and Practice 8: 317–320. doi:10.2147/AMEP.S133328. PMC PMC5422339. PMID 28496377. https://www.dovepress.com/letter-httpswwwdovepresscomadvances-in-medical-education-an-peer-reviewed-fulltext-article-AMEP.
- ↑ Zhang, Shan Yong; Zheng, Jia Wei; Yang, Chi; Zhang, Zhi Yuan; Shen, Guo Fang; Zhang, Jian Zhong; Xu, Yuan Jin; Cao, Xia (1 October 2012). "Case‐Based Learning in Clinical Courses in a Chinese College of Stomatology" (in en). Journal of Dental Education 76 (10): 1389–1392. doi:10.1002/j.0022-0337.2012.76.10.tb05396.x. ISSN 0022-0337. https://onlinelibrary.wiley.com/doi/10.1002/j.0022-0337.2012.76.10.tb05396.x.
Notes
This presentation is faithful to the original, with only a few minor changes to presentation, spelling, and grammar. In some cases important information was missing from the references, and that information was added.