Abstract
Background: Numerous validation studies in digital pathology confirmed its value as a diagnostic tool. However, a longer time to diagnosis than traditional microscopy has been seen as a significant barrier to the routine use of digital pathology. As a part of our validation study, we compared a digital and microscopic diagnostic time in the routine diagnostic setting.
Materials and methods: One senior staff pathologist reported 400 consecutive cases in histology, nongynecological, and fine needle aspiration cytology (20 sessions, 20 cases/session), over 4 weeks. Complex, difficult, and rare cases were excluded from the study to reduce the bias. A primary diagnosis was digital, followed by traditional microscopy, six months later, with only request forms available for both. Microscopic slides were scanned at ×20, digital images accessed through the fully integrated laboratory information management system (LIMS) and viewed in the image viewer on double 23” displays. A median broadband speed was 299 Mbps. A diagnostic time was measured from the point slides were made available to the point diagnosis was made or additional investigations were deemed necessary, recorded independently in minutes/session and compared.
Results: A digital diagnostic time was 1841 and microscopic 1956 min; digital being shorter than microscopic in 13 sessions. Four sessions with shorter microscopic diagnostic time included more cases requiring extensive use of magnifications over ×20. Diagnostic time was similar in three sessions.
Conclusions: A diagnostic time in digital pathology can be shorter than traditional microscopy in the routine diagnostic setting, with adequate and stable network speeds, fully integrated LIMS and double displays as default parameters. This also related to better ergonomics, larger viewing field, and absence of physical slide handling, with effects on both diagnostic and nondiagnostic time. Differences with previous studies included a design, image size, number of cases, specimen type, network speed, and participant's level of confidence and experience in digital reporting. Further advancements in working stations and gained experience in digital reporting are expected to improve diagnostic time and widen routine applications of digital pathology.
Keywords: Diagnostic time, digital pathology, turnaround
Introduction
Numerous validation studies in digital pathology confirmed its value as a diagnostic tool.[1][2][3] Main advantages for wider implementation of digital pathology, in comparison to traditional microscopy, include better ergonomics, immediate access to slides, and distance reporting. However, a longer time to diagnosis than traditional microscopy has been seen as a significant barrier to the routine use of digital pathology, especially in early studies.[4] Advances in working stations led to the narrowing or equaling of the diagnostic time gap and further improvements of the digital diagnostic experience, in experimental studies on a limited number of cases.[5][6][7][8] As a part of our validation study, we compared digital and microscopic diagnostic time in the routine diagnostic setting. Technical issues were seen as potential obstacles and shortened turnaround, through the faster digital diagnostic time, desired benefits.
Materials and methods
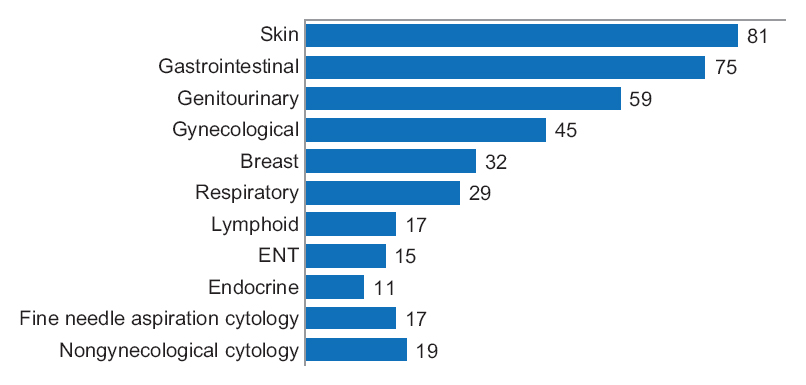
One senior staff pathologist reported 400 consecutive cases (1396 slides) in histology, nongynecological and fine needle aspiration cytology, by means of digital pathology and traditional microscopy (20 sessions and 20 cases/session), over four weeks [Figure 1].
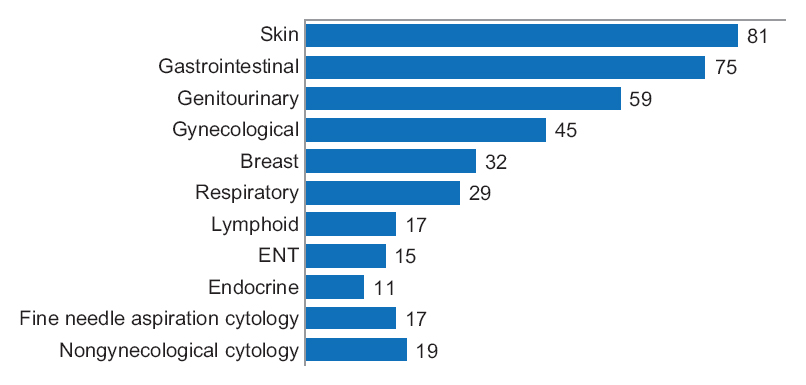
Figure 1. Case workload reported in this study
|
|
Complex, difficult, and rare cases were excluded from the study to reduce the bias, as pathologists often remember those cases for a long time. This group nevertheless included one complex, one difficult, and two rare cases. A primary diagnosis was digital, used for clinical management, followed by traditional microscopy, six months later. Only request forms were available for both primary and secondary diagnosis. Microscopic slides were prepared by standard techniques and routinely stained hematoxylin-eosin. In addition, upper gastrointestinal diagnostic biopsies were stained Alcian blue/periodic acid-Schiff and liver core biopsies Masson trichrome/iron/reticulin, respectively. Cytological slides were routinely stained either Romanowsky or Romanowsky/Papanicolaou and were not prescreened. Microscopic slides were scanned at ×20 using Scan Scope AT Turbo digital scanner (Leica). Digital images were accessed through the fully integrated laboratory information management system (LIMS) SymPathy (Tieto) and viewed in ImageScope (Leica) on a desktop PC with double displays [Table 1] using a broadband connection [Table 2].
| Table 1. Technical specification for equipment used in digital reporting
|
| Make and model
|
Dell OptiPlex 7010
|
| Operative system
|
Windows 7 Enterprise 64 bit
|
| Processor
|
i3-3240M 3.40 GHz
|
| Display size and resolution
|
Double 23", 1920x1200
|
| Read-only memory
|
500 GB
|
| Random access memory
|
8 GB
|
|
| Table 2. Broadband speed (Mbps) - variation, median and average
|
|
|
Variation
|
Median
|
Average
|
| Download speed
|
150–400
|
299
|
250
|
| Upload speed
|
35–150
|
55
|
50
|
|
A microscopic diagnosis was made on an Eclipse 80i light microscope (Nikon). Turnaround refers in this study to diagnostic (slide evaluation) and nondiagnostic time (dictation, sign off, access to clinical information, and previous history, etc.). A diagnostic time was measured from the point slides were made available to the point diagnosis was made or additional investigations were deemed necessary, recorded independently in minutes/session and compared. It did not include interruptions into the reporting sessions. An unstructured sessional log was recorded to identify factors contributing to improved diagnostic time. Broadband speeds were automatically recorded every 30 min into digital reporting sessions and analyzed.
Results
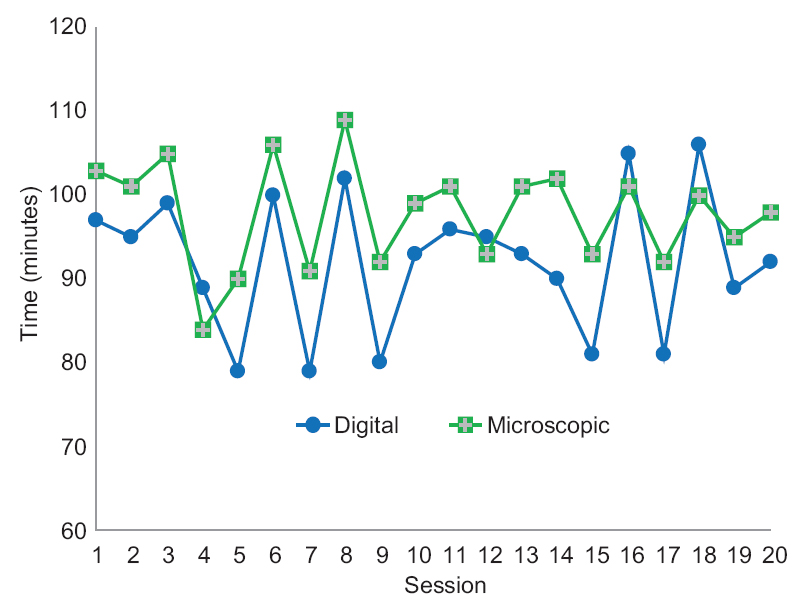
A total digital diagnostic time was shorter than microscopic, 1841 versus 1956 min, respectively. Distributions of digital and microscopic diagnostic time per session are shown in [Table 3] and [Figure 2].
| Table 3. Diagnostic time per session (min) - variation, median and average
|
|
|
Variation
|
Median
|
Average
|
| Digital
|
79–106
|
93
|
92.05
|
| Microscopic
|
84–109
|
99.5
|
97.8
|
|
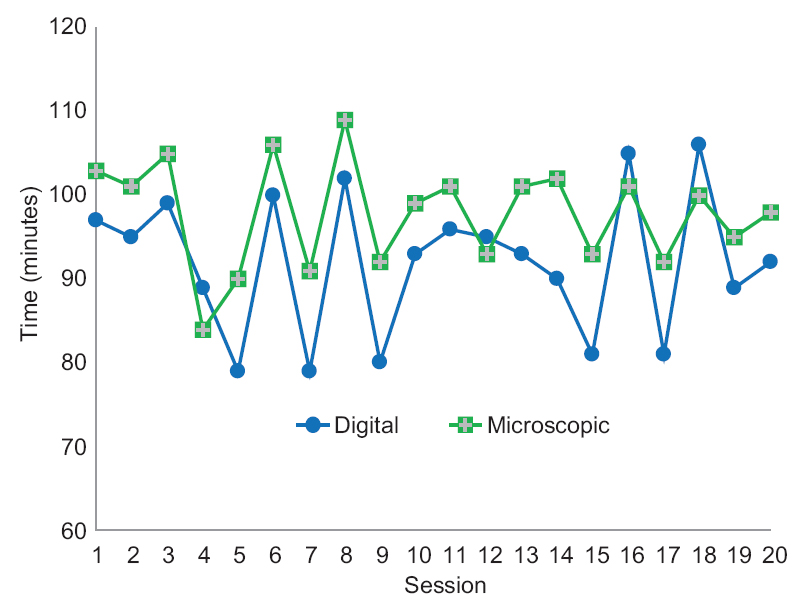
Figure 2. Distribution of diagnostic time
|
|
A digital diagnostic time was shorter than microscopic in 13 sessions. Four sessions with shorter microscopic diagnostic time included more cases requiring extensive use of magnifications over ×20 [Table 4].
| Table 4. Main reasons for more extensive use of magnification over ×20
|
| Reason
|
Diagnostic problem
|
| Low bacterial load
|
Presence of Helicobacter pylori
|
| Low tumour load
|
Presence of nonsmall cell cancer
|
| Nuclear features
|
Lymphoma versus carcinoma
|
|
The diagnostic time was similar in three sessions. Data analysis from the unstructured sessional log identified factors contributing most to the shorter digital diagnostic time [Table 5]. Differences with previous studies are listed in [Table 6].
| Table 5. Factors contributing to shortened digital diagnostic time
|
| Factors
|
Benefits
|
| Ergonomics
|
Less tiring reporting sessions
|
| Larger viewing field
|
Lesser number of viewing fields
|
| Absence of physical slide handling
|
Faster switching between slides/magnifications; reduced checking slides against requisitions
|
|
| Table 6. Differences with previous studies in digital reporting
|
| Variables
|
Previous studies
|
Present study
|
| Design
|
Experimental
|
Routine
|
| Network speed
|
Variable
|
Stable
|
| Image size
|
Scan at x20 and x40
|
Scan at x20
|
| Number of cases
|
Low
|
High
|
| Specimen type
|
Organ-specific
|
Mixed
|
| Experience
|
Variable
|
Long
|
|
Discussion
References
- ↑ Stathonikos, N.; Veta, M.; Huisman, A.; van Diest, P.J. (2013). "Going fully digital: Perspective of a Dutch academic pathology lab". Journal of Pathology Informatics 4: 15. doi:10.4103/2153-3539.114206. PMC PMC3709427. PMID 23858390. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3709427.
- ↑ Thorstenson, S.; Molin, J.; Lundström, C. (2014). "Implementation of large-scale routine diagnostics using whole slide imaging in Sweden: Digital pathology experiences 2006-2013". Journal of Pathology Informatics 5: 14. doi:10.4103/2153-3539.129452. PMC PMC4023034. PMID 24843825. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4023034.
- ↑ Bauer, T.W.; Slaw, R.J. (2014). "Validating whole-slide imaging for consultation diagnoses in surgical pathology". Archives of Pathology and Laboratory Medicine 138 (11): 1459-65. doi:10.5858/arpa.2013-0541-OA. PMID 24840034.
- ↑ Treanor, D.; Quirke, P. (2007). "The virtual slide and conventional microscope — A direct comparison of their diagnostic efficiency". The Journal of Pathology 213: 7a.
- ↑ Treanor, D.; Jordan-Owers, N.; Hodrien, J. et al.. "Virtual reality Powerwall versus conventional microscope for viewing pathology slides: An experimental comparison". Histopathology 55 (3): 294-300. doi:10.1111/j.1365-2559.2009.03389.x. PMID 19723144.
- ↑ Randell, R.; Ambepitiya, T.; Mello-Thoms, C. et al.. "Effect of display resolution on time to diagnosis with virtual pathology slides in a systematic search task". Journal of Digital Imaging 28 (1): 68–76. doi:10.1007/s10278-014-9726-8. PMC PMC4305057. PMID 25128321. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4305057.
- ↑ Randell, R.; Ruddle, R.A., Thomas, R.G. et al.. "Diagnosis of major cancer resection specimens with virtual slides: Impact of a novel digital pathology workstation". Human Pathology 45 (10): 2101–6. doi:10.1016/j.humpath.2014.06.017. PMID 25128229.
- ↑ Randell, R.; Ruddle, R.A., Mello-Thoms, C. et al.. "Virtual reality microscope versus conventional microscope regarding time to diagnosis: An experimental study". Histopathology 62 (2): 351-8. doi:10.1111/j.1365-2559.2012.04323.x. PMID 22882289.
Notes
This presentation is faithful to the original, with only a few minor changes to presentation. In some cases important information was missing from the references, and that information was added. Numbers 0 through 9 were changed from numerals to words when appropriate.