Difference between revisions of "Journal:Fostering reproducibility, reusability, and technology transfer in health informatics"
Shawndouglas (talk | contribs) (Saving and adding more.) |
Shawndouglas (talk | contribs) (Saving and adding more.) |
||
| Line 56: | Line 56: | ||
Once the outcome of this development is sufficiently mature and robust to be published and used in routine treatment or diagnosis, there is a need to transfer this knowledge to other research groups and, ultimately, clinical practice. Therefore, a straightforward technology transfer to a manufacturer of [[medical device]]s would be beneficial.<ref name=":0">{{Cite journal |last=Brito |first=Jaqueline J |last2=Li |first2=Jun |last3=Moore |first3=Jason H |last4=Greene |first4=Casey S |last5=Nogoy |first5=Nicole A |last6=Garmire |first6=Lana X |last7=Mangul |first7=Serghei |date=2020-06-01 |title=Recommendations to enhance rigor and reproducibility in biomedical research |url=https://academic.oup.com/gigascience/article/doi/10.1093/gigascience/giaa056/5849489 |journal=GigaScience |language=en |volume=9 |issue=6 |pages=giaa056 |doi=10.1093/gigascience/giaa056 |issn=2047-217X |pmc=PMC7263079 |pmid=32479592}}</ref><ref name=":2">{{Cite journal |last=Riemenschneider |first=Mona |last2=Wienbeck |first2=Joachim |last3=Scherag |first3=André |last4=Heider |first4=Dominik |date=2018-06 |title=Data Science for Molecular Diagnostics Applications: From Academia to Clinic to Industry |url=http://www.liebertpub.com/doi/10.1089/sysm.2018.0002 |journal=Systems Medicine |language=en |volume=1 |issue=1 |pages=13–17 |doi=10.1089/sysm.2018.0002 |issn=2573-3370}}</ref> | Once the outcome of this development is sufficiently mature and robust to be published and used in routine treatment or diagnosis, there is a need to transfer this knowledge to other research groups and, ultimately, clinical practice. Therefore, a straightforward technology transfer to a manufacturer of [[medical device]]s would be beneficial.<ref name=":0">{{Cite journal |last=Brito |first=Jaqueline J |last2=Li |first2=Jun |last3=Moore |first3=Jason H |last4=Greene |first4=Casey S |last5=Nogoy |first5=Nicole A |last6=Garmire |first6=Lana X |last7=Mangul |first7=Serghei |date=2020-06-01 |title=Recommendations to enhance rigor and reproducibility in biomedical research |url=https://academic.oup.com/gigascience/article/doi/10.1093/gigascience/giaa056/5849489 |journal=GigaScience |language=en |volume=9 |issue=6 |pages=giaa056 |doi=10.1093/gigascience/giaa056 |issn=2047-217X |pmc=PMC7263079 |pmid=32479592}}</ref><ref name=":2">{{Cite journal |last=Riemenschneider |first=Mona |last2=Wienbeck |first2=Joachim |last3=Scherag |first3=André |last4=Heider |first4=Dominik |date=2018-06 |title=Data Science for Molecular Diagnostics Applications: From Academia to Clinic to Industry |url=http://www.liebertpub.com/doi/10.1089/sysm.2018.0002 |journal=Systems Medicine |language=en |volume=1 |issue=1 |pages=13–17 |doi=10.1089/sysm.2018.0002 |issn=2573-3370}}</ref> | ||
==Challenges of scientific software development for health== | ===Challenges of scientific software development for health=== | ||
While the knowledge and technologies to develop effective and efficacious AI-driven [[clinical decision support system]]s exist, a manifold of pressing issues hinders further reuse in research and transfer to clinical practice. In software development projects in the industry, specialized developers typically work in large teams with considerable resources and are able to focus on usability and reusability.<ref>{{Cite journal |last=Guellec, D.; van Pottelsberghe de la Potterie, B. |date=2000-06-14 |title=The Impact of Public R&D Expenditure on Business R&D |url=https://www.oecd-ilibrary.org/science-and-technology/the-impact-of-public-r-d-expenditure-on-business-r-d_670385851815 |journal=OECD Science, Technology and Industry Working Papers |language=en |volume=2000/04 |issue= |doi=10.1787/670385851815}}</ref><ref name=":1">{{Cite journal |last=Mangul |first=Serghei |last2=Mosqueiro |first2=Thiago |last3=Abdill |first3=Richard J. |last4=Duong |first4=Dat |last5=Mitchell |first5=Keith |last6=Sarwal |first6=Varuni |last7=Hill |first7=Brian |last8=Brito |first8=Jaqueline |last9=Littman |first9=Russell Jared |last10=Statz |first10=Benjamin |last11=Lam |first11=Angela Ka-Mei |date=2019-06-20 |title=Challenges and recommendations to improve the installability and archival stability of omics computational tools |url=https://dx.plos.org/10.1371/journal.pbio.3000333 |journal=PLOS Biology |language=en |volume=17 |issue=6 |pages=e3000333 |doi=10.1371/journal.pbio.3000333 |issn=1545-7885 |pmc=PMC6605654 |pmid=31220077}}</ref> In contrast, academic teams often consist of small groups of researchers (e.g., graduate students and postdoctoral scholars) who are typically not trained software engineers and only have temporary contracts and frequent turnover. Thus, individuals often develop software on a one-person-one-project basis.<ref name=":0" /><ref name=":1" /> | While the knowledge and technologies to develop effective and efficacious AI-driven [[clinical decision support system]]s exist, a manifold of pressing issues hinders further reuse in research and transfer to clinical practice. In software development projects in the industry, specialized developers typically work in large teams with considerable resources and are able to focus on usability and reusability.<ref>{{Cite journal |last=Guellec, D.; van Pottelsberghe de la Potterie, B. |date=2000-06-14 |title=The Impact of Public R&D Expenditure on Business R&D |url=https://www.oecd-ilibrary.org/science-and-technology/the-impact-of-public-r-d-expenditure-on-business-r-d_670385851815 |journal=OECD Science, Technology and Industry Working Papers |language=en |volume=2000/04 |issue= |doi=10.1787/670385851815}}</ref><ref name=":1">{{Cite journal |last=Mangul |first=Serghei |last2=Mosqueiro |first2=Thiago |last3=Abdill |first3=Richard J. |last4=Duong |first4=Dat |last5=Mitchell |first5=Keith |last6=Sarwal |first6=Varuni |last7=Hill |first7=Brian |last8=Brito |first8=Jaqueline |last9=Littman |first9=Russell Jared |last10=Statz |first10=Benjamin |last11=Lam |first11=Angela Ka-Mei |date=2019-06-20 |title=Challenges and recommendations to improve the installability and archival stability of omics computational tools |url=https://dx.plos.org/10.1371/journal.pbio.3000333 |journal=PLOS Biology |language=en |volume=17 |issue=6 |pages=e3000333 |doi=10.1371/journal.pbio.3000333 |issn=1545-7885 |pmc=PMC6605654 |pmid=31220077}}</ref> In contrast, academic teams often consist of small groups of researchers (e.g., graduate students and postdoctoral scholars) who are typically not trained software engineers and only have temporary contracts and frequent turnover. Thus, individuals often develop software on a one-person-one-project basis.<ref name=":0" /><ref name=":1" /> | ||
Moreover, funders and the academic hiring and promotion processes incentivize the pressure to publish and focus on “novelty” rather than software quality. Thus, it entices researchers to focus on theoretical aspects and proof of concept development.<ref name=":0" /><ref>{{Cite journal |last=Mangul |first=Serghei |last2=Martin |first2=Lana S. |last3=Eskin |first3=Eleazar |last4=Blekhman |first4=Ran |date=2019-12 |title=Improving the usability and archival stability of bioinformatics software |url=https://genomebiology.biomedcentral.com/articles/10.1186/s13059-019-1649-8 |journal=Genome Biology |language=en |volume=20 |issue=1 |pages=47, s13059–019–1649-8 |doi=10.1186/s13059-019-1649-8 |issn=1474-760X |pmc=PMC6391762 |pmid=30813962}}</ref> Therefore, most researchers implement software in a prototype-centered manner, which often lacks [[Quality (business)|quality]] checks such as systematic testing and may be published quickly.<ref name=":3">{{Cite journal |last=Lee |first=Graham |last2=Bacon |first2=Sebastian |last3=Bush |first3=Ian |last4=Fortunato |first4=Laura |last5=Gavaghan |first5=David |last6=Lestang |first6=Thibault |last7=Morton |first7=Caroline |last8=Robinson |first8=Martin |last9=Rocca-Serra |first9=Philippe |last10=Sansone |first10=Susanna-Assunta |last11=Webb |first11=Helena |date=2021-02 |title=Barely sufficient practices in scientific computing |url=https://linkinghub.elsevier.com/retrieve/pii/S2666389921000167 |journal=Patterns |language=en |volume=2 |issue=2 |pages=100206 |doi=10.1016/j.patter.2021.100206 |pmc=PMC7892476 |pmid=33659915}}</ref> However, these implementations often lack crucial qualities required for long-term reuse, such as documentation, usability, appropriate performance for real-life application, user-friendly interfaces, reusability, or minimized risk for potential users.<ref name=":0" /><ref name=":2" /> | Moreover, funders and the academic hiring and promotion processes incentivize the pressure to publish and focus on “novelty” rather than software quality. Thus, it entices researchers to focus on theoretical aspects and proof of concept development.<ref name=":0" /><ref name=":9">{{Cite journal |last=Mangul |first=Serghei |last2=Martin |first2=Lana S. |last3=Eskin |first3=Eleazar |last4=Blekhman |first4=Ran |date=2019-12 |title=Improving the usability and archival stability of bioinformatics software |url=https://genomebiology.biomedcentral.com/articles/10.1186/s13059-019-1649-8 |journal=Genome Biology |language=en |volume=20 |issue=1 |pages=47, s13059–019–1649-8 |doi=10.1186/s13059-019-1649-8 |issn=1474-760X |pmc=PMC6391762 |pmid=30813962}}</ref> Therefore, most researchers implement software in a prototype-centered manner, which often lacks [[Quality (business)|quality]] checks such as systematic testing and may be published quickly.<ref name=":3">{{Cite journal |last=Lee |first=Graham |last2=Bacon |first2=Sebastian |last3=Bush |first3=Ian |last4=Fortunato |first4=Laura |last5=Gavaghan |first5=David |last6=Lestang |first6=Thibault |last7=Morton |first7=Caroline |last8=Robinson |first8=Martin |last9=Rocca-Serra |first9=Philippe |last10=Sansone |first10=Susanna-Assunta |last11=Webb |first11=Helena |date=2021-02 |title=Barely sufficient practices in scientific computing |url=https://linkinghub.elsevier.com/retrieve/pii/S2666389921000167 |journal=Patterns |language=en |volume=2 |issue=2 |pages=100206 |doi=10.1016/j.patter.2021.100206 |pmc=PMC7892476 |pmid=33659915}}</ref> However, these implementations often lack crucial qualities required for long-term reuse, such as documentation, usability, appropriate performance for real-life application, user-friendly interfaces, reusability, or minimized risk for potential users.<ref name=":0" /><ref name=":2" /> | ||
Recently, scientific journals such as ''GigaScience'' or ''Biostatistics'' have promoted reproducibility and reusability by mandating FAIR principles (findability, accessibility, interoperability, and reusability). The concept of FAIR establishes a guideline for scientific data management and documentation.<ref name=":0" /><ref>{{Cite journal |last=Wilkinson |first=Mark D. |last2=Dumontier |first2=Michel |last3=Aalbersberg |first3=IJsbrand Jan |last4=Appleton |first4=Gabrielle |last5=Axton |first5=Myles |last6=Baak |first6=Arie |last7=Blomberg |first7=Niklas |last8=Boiten |first8=Jan-Willem |last9=da Silva Santos |first9=Luiz Bonino |last10=Bourne |first10=Philip E. |last11=Bouwman |first11=Jildau |date=2016-12 |title=The FAIR Guiding Principles for scientific data management and stewardship |url=http://www.nature.com/articles/sdata201618 |journal=Scientific Data |language=en |volume=3 |issue=1 |pages=160018 |doi=10.1038/sdata.2016.18 |issn=2052-4463 |pmc=PMC4792175 |pmid=26978244}}</ref> | Recently, scientific journals such as ''GigaScience'' or ''Biostatistics'' have promoted reproducibility and reusability by mandating FAIR principles (findability, accessibility, interoperability, and reusability). The concept of FAIR establishes a guideline for scientific data management and documentation.<ref name=":0" /><ref>{{Cite journal |last=Wilkinson |first=Mark D. |last2=Dumontier |first2=Michel |last3=Aalbersberg |first3=IJsbrand Jan |last4=Appleton |first4=Gabrielle |last5=Axton |first5=Myles |last6=Baak |first6=Arie |last7=Blomberg |first7=Niklas |last8=Boiten |first8=Jan-Willem |last9=da Silva Santos |first9=Luiz Bonino |last10=Bourne |first10=Philip E. |last11=Bouwman |first11=Jildau |date=2016-12 |title=The FAIR Guiding Principles for scientific data management and stewardship |url=http://www.nature.com/articles/sdata201618 |journal=Scientific Data |language=en |volume=3 |issue=1 |pages=160018 |doi=10.1038/sdata.2016.18 |issn=2052-4463 |pmc=PMC4792175 |pmid=26978244}}</ref> | ||
| Line 70: | Line 70: | ||
Additionally, modern systems medicine approaches integrate all facets of private data such as [[electronic health record]]s (EHR)<ref>{{Cite journal |last=Shickel |first=Benjamin |last2=Tighe |first2=Patrick James |last3=Bihorac |first3=Azra |last4=Rashidi |first4=Parisa |date=2018-09 |title=Deep EHR: A Survey of Recent Advances in Deep Learning Techniques for Electronic Health Record (EHR) Analysis |url=https://ieeexplore.ieee.org/document/8086133/ |journal=IEEE Journal of Biomedical and Health Informatics |volume=22 |issue=5 |pages=1589–1604 |doi=10.1109/JBHI.2017.2767063 |issn=2168-2194 |pmc=PMC6043423 |pmid=29989977}}</ref>, [[laboratory]] results<ref>{{Cite journal |last=Goecks |first=Jeremy |last2=Jalili |first2=Vahid |last3=Heiser |first3=Laura M. |last4=Gray |first4=Joe W. |date=2020-04 |title=How Machine Learning Will Transform Biomedicine |url=https://linkinghub.elsevier.com/retrieve/pii/S0092867420302841 |journal=Cell |language=en |volume=181 |issue=1 |pages=92–101 |doi=10.1016/j.cell.2020.03.022 |pmc=PMC7141410 |pmid=32243801}}</ref>, [[medical imaging]]<ref>{{Cite journal |last=Anwar |first=Syed Muhammad |last2=Majid |first2=Muhammad |last3=Qayyum |first3=Adnan |last4=Awais |first4=Muhammad |last5=Alnowami |first5=Majdi |last6=Khan |first6=Muhammad Khurram |date=2018-11 |title=Medical Image Analysis using Convolutional Neural Networks: A Review |url=http://link.springer.com/10.1007/s10916-018-1088-1 |journal=Journal of Medical Systems |language=en |volume=42 |issue=11 |pages=226 |doi=10.1007/s10916-018-1088-1 |issn=0148-5598}}</ref>, omics resources such as the cancer genome atlas (TCGA) or the gene expression omnibus<ref name=":6" /><ref name=":7" /><ref>{{Citation |last=Clough |first=Emily |last2=Barrett |first2=Tanya |date=2016 |editor-last=Mathé |editor-first=Ewy |editor2-last=Davis |editor2-first=Sean |title=The Gene Expression Omnibus Database |url=http://link.springer.com/10.1007/978-1-4939-3578-9_5 |work=Statistical Genomics |publisher=Springer New York |place=New York, NY |volume=1418 |pages=93–110 |doi=10.1007/978-1-4939-3578-9_5 |isbn=978-1-4939-3576-5 |pmc=PMC4944384 |pmid=27008011 |access-date=2021-08-22}}</ref><ref>{{Cite journal |last=Tomczak |first=Katarzyna |last2=Czerwińska |first2=Patrycja |last3=Wiznerowicz |first3=Maciej |date=2015 |title=The Cancer Genome Atlas (TCGA): An immeasurable source of knowledge |url=http://www.termedia.pl/doi/10.5114/wo.2014.47136 |journal=Współczesna Onkologia |volume=1A |pages=68–77 |doi=10.5114/wo.2014.47136 |issn=1428-2526 |pmc=PMC4322527 |pmid=25691825}}</ref>, or pathway information.<ref name=":5" /><ref name=":7" /><ref name=":8" /> However, sensitive patient data that enables an association of confidential personal information to single individuals underlies strict regulations such as the European [[General Data Protection Regulation]] (GDPR).<ref>{{Cite book |last=Voigt |first=Paul |last2=von dem Bussche |first2=Axel |date=2017 |title=The EU General Data Protection Regulation (GDPR) |url=http://link.springer.com/10.1007/978-3-319-57959-7 |language=en |publisher=Springer International Publishing |place=Cham |doi=10.1007/978-3-319-57959-7 |isbn=978-3-319-57958-0}}</ref> Therefore, the exchange within and among institutes is perceived as insurmountable, posing a roadblock hampering significant data-based medical innovations. | Additionally, modern systems medicine approaches integrate all facets of private data such as [[electronic health record]]s (EHR)<ref>{{Cite journal |last=Shickel |first=Benjamin |last2=Tighe |first2=Patrick James |last3=Bihorac |first3=Azra |last4=Rashidi |first4=Parisa |date=2018-09 |title=Deep EHR: A Survey of Recent Advances in Deep Learning Techniques for Electronic Health Record (EHR) Analysis |url=https://ieeexplore.ieee.org/document/8086133/ |journal=IEEE Journal of Biomedical and Health Informatics |volume=22 |issue=5 |pages=1589–1604 |doi=10.1109/JBHI.2017.2767063 |issn=2168-2194 |pmc=PMC6043423 |pmid=29989977}}</ref>, [[laboratory]] results<ref>{{Cite journal |last=Goecks |first=Jeremy |last2=Jalili |first2=Vahid |last3=Heiser |first3=Laura M. |last4=Gray |first4=Joe W. |date=2020-04 |title=How Machine Learning Will Transform Biomedicine |url=https://linkinghub.elsevier.com/retrieve/pii/S0092867420302841 |journal=Cell |language=en |volume=181 |issue=1 |pages=92–101 |doi=10.1016/j.cell.2020.03.022 |pmc=PMC7141410 |pmid=32243801}}</ref>, [[medical imaging]]<ref>{{Cite journal |last=Anwar |first=Syed Muhammad |last2=Majid |first2=Muhammad |last3=Qayyum |first3=Adnan |last4=Awais |first4=Muhammad |last5=Alnowami |first5=Majdi |last6=Khan |first6=Muhammad Khurram |date=2018-11 |title=Medical Image Analysis using Convolutional Neural Networks: A Review |url=http://link.springer.com/10.1007/s10916-018-1088-1 |journal=Journal of Medical Systems |language=en |volume=42 |issue=11 |pages=226 |doi=10.1007/s10916-018-1088-1 |issn=0148-5598}}</ref>, omics resources such as the cancer genome atlas (TCGA) or the gene expression omnibus<ref name=":6" /><ref name=":7" /><ref>{{Citation |last=Clough |first=Emily |last2=Barrett |first2=Tanya |date=2016 |editor-last=Mathé |editor-first=Ewy |editor2-last=Davis |editor2-first=Sean |title=The Gene Expression Omnibus Database |url=http://link.springer.com/10.1007/978-1-4939-3578-9_5 |work=Statistical Genomics |publisher=Springer New York |place=New York, NY |volume=1418 |pages=93–110 |doi=10.1007/978-1-4939-3578-9_5 |isbn=978-1-4939-3576-5 |pmc=PMC4944384 |pmid=27008011 |access-date=2021-08-22}}</ref><ref>{{Cite journal |last=Tomczak |first=Katarzyna |last2=Czerwińska |first2=Patrycja |last3=Wiznerowicz |first3=Maciej |date=2015 |title=The Cancer Genome Atlas (TCGA): An immeasurable source of knowledge |url=http://www.termedia.pl/doi/10.5114/wo.2014.47136 |journal=Współczesna Onkologia |volume=1A |pages=68–77 |doi=10.5114/wo.2014.47136 |issn=1428-2526 |pmc=PMC4322527 |pmid=25691825}}</ref>, or pathway information.<ref name=":5" /><ref name=":7" /><ref name=":8" /> However, sensitive patient data that enables an association of confidential personal information to single individuals underlies strict regulations such as the European [[General Data Protection Regulation]] (GDPR).<ref>{{Cite book |last=Voigt |first=Paul |last2=von dem Bussche |first2=Axel |date=2017 |title=The EU General Data Protection Regulation (GDPR) |url=http://link.springer.com/10.1007/978-3-319-57959-7 |language=en |publisher=Springer International Publishing |place=Cham |doi=10.1007/978-3-319-57959-7 |isbn=978-3-319-57958-0}}</ref> Therefore, the exchange within and among institutes is perceived as insurmountable, posing a roadblock hampering significant data-based medical innovations. | ||
===Quality management=== | |||
The design and development of [[medical device]]s used in clinical practice, including software as a medical device, have to comply with regulations and standards that ensure the safety and quality of medical devices worldwide.<ref>{{Cite journal |last=Maak |first=Travis G. |last2=Wylie |first2=James D. |date=2016-08 |title=Medical Device Regulation: A Comparison of the United States and the European Union |url=http://journals.lww.com/00124635-201608000-00004 |journal=Journal of the American Academy of Orthopaedic Surgeons |language=en |volume=24 |issue=8 |pages=537–543 |doi=10.5435/JAAOS-D-15-00403 |issn=1067-151X}}</ref><ref>{{Cite book |date=2011 |editor-last=World Health Organization |title=Development of medical device policies |series=WHO medical device technical series |publisher=World Health Organization |place=Geneva, Switzerland |isbn=978-92-4-150163-7}}</ref> These regulations include standards concerning quality management (QM), the software development life cycle (including agile methods such as Scrum<ref>{{Cite book |last=Schwaber |first=Ken |last2=Beedle |first2=Mike |date=2002 |title=Agile software development with Scrum |series=Series in agile software development |publisher=Prentice Hall |place=Upper Saddle River, NJ |isbn=978-0-13-067634-4}}</ref> or Kanban<ref>{{Cite book |last=Anderson |first=David J. |date=2010 |title=Kanban: Successful evolutionary change for your technology business |url=https://www.worldcat.org/title/mediawiki/oclc/699604917 |publisher=Blue Hole Press |place=Sequim, Washington |isbn=978-0-9845214-0-1 |oclc=699604917}}</ref>), and [[risk management]]. However, such measures are not yet a standard in academic research work.<ref name=":1" /><ref name=":9" /><ref>{{Cite journal |last=Zamith |first=Manuel |last2=Gonçalves |first2=Gil |date=2018 |title=Towards an Agile Development Model for Certifiable Medical Device Software - Taking Advantage of the Medical Device Regulation: |url=http://www.scitepress.org/DigitalLibrary/Link.aspx?doi=10.5220/0006861301320140 |journal=Proceedings of the 13th International Conference on Software Technologies |publisher=SCITEPRESS - Science and Technology Publications |place=Porto, Portugal |pages=132–140 |doi=10.5220/0006861301320140 |isbn=978-989-758-320-9}}</ref> | |||
The challenges in academic development procedures, as described before, affect technology transfer as well as reproducibility and reusability among researchers, as well as to the industry. It is usually restricted to transferring an intellectual method and know-how while discarding all created artifacts (e.g., documents for development planning and software code). In particular, manufacturers will need to understand the principles of the new method, train their staff members, and maintain design and development records when creating the final product. The record will include design documents, meeting minutes, and other documents produced during the development. This effort causes a significant overhead in the time and work they have to invest before the product is ready for the market.<ref>{{Cite journal |last=Sharma |first=Arjun |last2=Blank |first2=Anthony |last3=Patel |first3=Parashar |last4=Stein |first4=Kenneth |date=2013-03 |title=Health care policy and regulatory implications on medical device innovations: A cardiac rhythm medical device industry perspective |url=http://link.springer.com/10.1007/s10840-013-9781-y |journal=Journal of Interventional Cardiac Electrophysiology |language=en |volume=36 |issue=2 |pages=107–117 |doi=10.1007/s10840-013-9781-y |issn=1383-875X |pmc=PMC3606523 |pmid=23474980}}</ref> | |||
Introducing [[quality management system]]s (QMS) by industry has proven to guarantee continuous high quality among projects and procedures within an organization. Our goal is to facilitate this experience in academic environments. Establishing an academia-tailored QMS for research organizations can address the described challenges of software quality, documentation, accessibility, traceability, and reproducibility and help software development in research organizations reach higher quality and standards. These quality standards are particularly critical for software that is intended to be used in the medical context. We can significantly reduce software transfer barriers among researchers in academia and industry if these standards are established from the start. | |||
Moreover, it has the potential to facilitate and speed up the transfer to clinical practice and thereby improve medical diagnosis or treatment of patients rapidly. However, our recommendations are based on standards that are common for medical device development but do not have the intention to shortcut any steps of the regular medical device development; this will always have to be done according to the strict rules and regulations that apply. Other benefits of a QMS for medical device development are also beneficial for research organizations when developing such software, including making responsibilities clearer, phasing in new team members quickly, and ensuring everyone knows how their work contributes to project and organizational goals. | |||
Requirements for QM are defined in [[ISO 9000|ISO 9001]]<ref name="ISO9001">{{cite web |url=https://www.iso.org/standard/62085.html |title=ISO 9001:2015 Quality management systems — Requirements |publisher=International Organization for Standardization |date=September 2015}}</ref>, in [[ISO 13485]]<ref name="ISO13485">{{cite web |url=https://www.iso.org/standard/59752.html |title=ISO 13485:2016 | |||
Medical devices — Quality management systems — Requirements for regulatory purposes |publisher=International Organization for Standardization |date=March 2016}}</ref>, and the [[21 CFR Part 11|Code of Federal Regulation (CFR) Title 21]].<ref name="FDA_CFRTitle21">{{cite web |url=https://www.accessdata.fda.gov/scripts/cdrh/cfdocs/cfcfr/cfrsearch.cfm |title=CFR - Code of Federal Regulations Title 21 |publisher=U.S. Food and Drug Administration |date=01 April 2020}}</ref> However, while ISO 9001 is generic and can be used in different fields, ISO 13485 is specific for QM in medical device development. The main differences are that ISO 9001 requires the organization to demonstrate [[Continual improvement process|continual improvement]]. In contrast, ISO 13485 only requires the certified organization to verify that the QMS is effectively implemented and maintained. Additionally, ISO 9001 includes customer satisfaction, which is not relevant to ISO 13485. There are also some other differences in ISO 13485, e.g., that the promotion and awareness of regulatory requirements is a management responsibility, that risk assessment and management need to be carried out (according to [[ISO 14971]]), and some others. Unfortunately, ISO 13485 is most likely outside of what is feasible for research groups in universities and other research organizations. | |||
===Our goal: Academia-tailored QMS=== | |||
Until now, there has been no guidance on how to establish an academia-tailored QMS for research organizations that balances between not having any QMS at all and a wholly formulated QMS that complies with official regulatory standards. Here, we present a synopsis of relevant requirements in such standards and adjust these toward software development requirements in academia. We aim to embrace the benefits and facilitate the technology transfer as much as possible while keeping the overhead for researchers and developers in a well manageable range. Thus, we tailor the content for use in universities or similar research organizations that focus on software in the medical setting. | |||
However, the ideas presented here do not provide a shortcut when developing medical software. Any development of medical software must strictly follow the relevant regulations in the specific country or region. Therefore, our suggestions provide a starting point intended to be adapted to specific requirements as needed and we refer to it as MDx-ready (i.e., ready for transferring it into [[molecular diagnostics]] SaMD implementations). This flexibility is well in the mindset of most QMS: If there is a profound reason for the change, change it, but consider all relevant aspects and document the reasons and the changes. | |||
==QMS for medical software research== | |||
==References== | ==References== | ||
Revision as of 19:56, 22 August 2021
| Full article title | Fostering reproducibility, reusability, and technology transfer in health informatics |
|---|---|
| Journal | iScience |
| Author(s) | Hauschild, Anne-Christin; Eick, Lisa; Wienbeck, Joachim; Heider, Dominik |
| Author affiliation(s) | Philipps University of Marburg |
| Primary contact | Email: dominik dot heider at uni-marburg dot de |
| Year published | 2021 |
| Volume and issue | 24(7) |
| Article # | 102803 |
| DOI | 10.1016/j.isci.2021.102803 |
| ISSN | 2589-0042 |
| Distribution license | Creative Commons Attribution 4.0 International |
| Website | https://www.sciencedirect.com/science/article/pii/S2589004221007719 |
| Download | https://www.sciencedirect.com/science/article/pii/S2589004221007719/pdfft (PDF) |
|
|
This article should be considered a work in progress and incomplete. Consider this article incomplete until this notice is removed. |
Abstract
Computational methods can transform healthcare. In particular, health informatics combined with artificial intelligence (AI) has shown tremendous potential when applied in various fields of medical research and has opened a new era for precision medicine. The development of reusable biomedical software for research or clinical practice is time-consuming and requires rigorous compliance with quality requirements as defined by international standards.
However, research projects rarely implement such measures, hindering smooth technology transfer to the research community or manufacturers, as well as reproducibility and reusability.
Here, we present a guideline for quality management systems (QMS) for academic organizations incorporating the essential components, while confining the requirements to an easily manageable effort. It provides a starting point to effortlessly implement a QMS tailored to specific needs and greatly facilitates technology transfer in a controlled manner, thereby supporting reproducibility and reusability.
Ultimately, the emerging standardized workflows can pave the way for an accelerated deployment in clinical practice.
Keywords: health informatics, bioinformatics, software engineering, software robustness
|
Introduction
Computational approaches offer new opportunities to transform health care. In particular, modern artificial intelligence (AI) and machine learning (ML) techniques have shown substantial potential when applied in various fields of medical research and therefore have opened up a new era for precision medicine. (Hawgood et al., 2015)[1] In the last decade, universities and other research organizations supported and encouraged by public funding agencies have allocated tremendous efforts to develop and enhance such predictive software models, algorithms, and “systems as medical devices” (SaMD) for clinical research and application.
A manifold of studies have proven AI to be advantageous for disease diagnosis, prognosis, and disease monitoring.[2][3] In cancer research, for instance, ML is used on omics data to gain deeper insights and understanding of the genetic and metabolic alterations that determine disease progression and enable tailored prognoses and monitoring.[4][5][6][7] Additionally, computational models on clinical information are used to assess individualized health risks, for instance, to identify high-risk patients for sepsis in intensive care units[8][9], the analysis of longitudinal data for the early detection of heart failure[10], or applications in infectious diseases.[11][12]
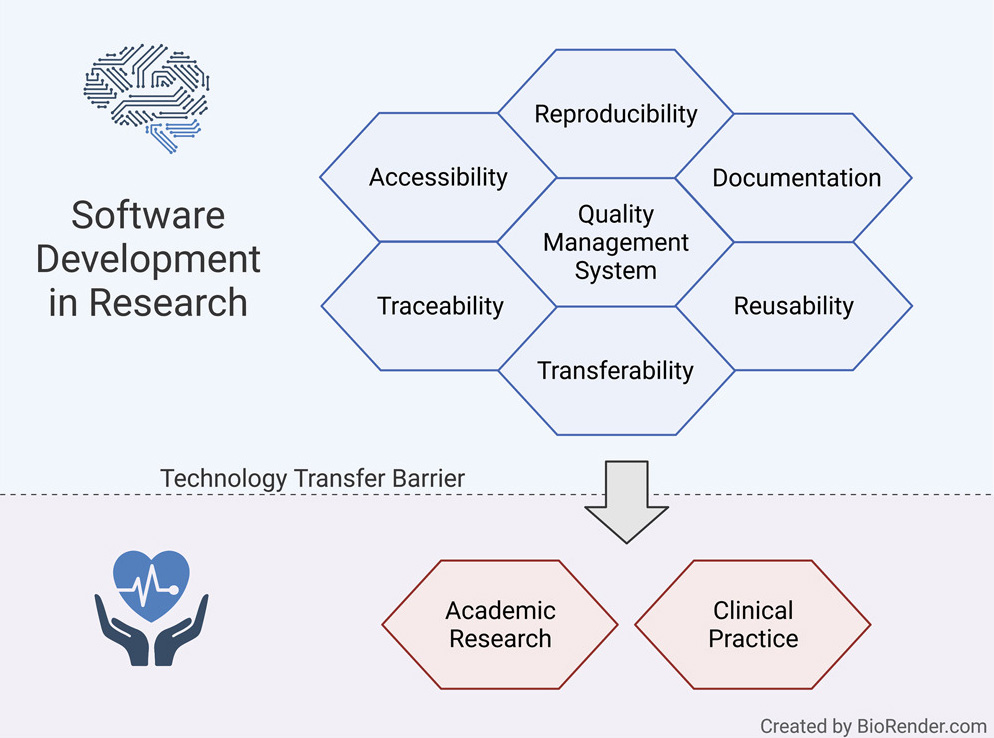
Once the outcome of this development is sufficiently mature and robust to be published and used in routine treatment or diagnosis, there is a need to transfer this knowledge to other research groups and, ultimately, clinical practice. Therefore, a straightforward technology transfer to a manufacturer of medical devices would be beneficial.[13][14]
Challenges of scientific software development for health
While the knowledge and technologies to develop effective and efficacious AI-driven clinical decision support systems exist, a manifold of pressing issues hinders further reuse in research and transfer to clinical practice. In software development projects in the industry, specialized developers typically work in large teams with considerable resources and are able to focus on usability and reusability.[15][16] In contrast, academic teams often consist of small groups of researchers (e.g., graduate students and postdoctoral scholars) who are typically not trained software engineers and only have temporary contracts and frequent turnover. Thus, individuals often develop software on a one-person-one-project basis.[13][16]
Moreover, funders and the academic hiring and promotion processes incentivize the pressure to publish and focus on “novelty” rather than software quality. Thus, it entices researchers to focus on theoretical aspects and proof of concept development.[13][17] Therefore, most researchers implement software in a prototype-centered manner, which often lacks quality checks such as systematic testing and may be published quickly.[18] However, these implementations often lack crucial qualities required for long-term reuse, such as documentation, usability, appropriate performance for real-life application, user-friendly interfaces, reusability, or minimized risk for potential users.[13][14]
Recently, scientific journals such as GigaScience or Biostatistics have promoted reproducibility and reusability by mandating FAIR principles (findability, accessibility, interoperability, and reusability). The concept of FAIR establishes a guideline for scientific data management and documentation.[13][19]
However, as recently surveyed by Pinto et al.[20], documentation of scientific software is one of the most significant “pain points.”[20] Journal publications are typically the primary source of documentation for scientific software and are quickly outdated by the agile software development style in academia.[16] Ideally, documentation should be detailed enough so that a developer with no prior knowledge of the project should make productive use of the software and use it for further development without biases or limitations.[13][18]
Another critical factor is accessibility. A lack of strict enforcement by journals, organizations, and funders has resulted in a loss of crucial data and software code.[13] According to an extensive analysis by Mangul et al., almost 28% of all resources linked in publications were not accessible, indicating poor maintenance. Moreover, a large proportion of software tested by Mangul et al. was not usable due to non-installability or lack of portability. The main inhibitors were storage locations outside of the journal’s directories or public versioning systems.[16][18]
Reproducibility and traceability are two of the most important aspects of biomedical and health informatics.[18][21] The lack of publicly available and comprehensible source code undermines the auditing of published methods and results. Additionally, the traceability of changes via version control is critical for reproducibility and reuse of research and code that replicators get to use.[18] These aspects ultimately undermine scientific rigor, transparency, and reproducibility.[13] The previously described accessibility, documentation, portability, and reusability factors are essential to ensure reproducibility and underpin trust in the scientific record of scientific software.[18]
Additionally, modern systems medicine approaches integrate all facets of private data such as electronic health records (EHR)[22], laboratory results[23], medical imaging[24], omics resources such as the cancer genome atlas (TCGA) or the gene expression omnibus[5][6][25][26], or pathway information.[4][6][7] However, sensitive patient data that enables an association of confidential personal information to single individuals underlies strict regulations such as the European General Data Protection Regulation (GDPR).[27] Therefore, the exchange within and among institutes is perceived as insurmountable, posing a roadblock hampering significant data-based medical innovations.
Quality management
The design and development of medical devices used in clinical practice, including software as a medical device, have to comply with regulations and standards that ensure the safety and quality of medical devices worldwide.[28][29] These regulations include standards concerning quality management (QM), the software development life cycle (including agile methods such as Scrum[30] or Kanban[31]), and risk management. However, such measures are not yet a standard in academic research work.[16][17][32]
The challenges in academic development procedures, as described before, affect technology transfer as well as reproducibility and reusability among researchers, as well as to the industry. It is usually restricted to transferring an intellectual method and know-how while discarding all created artifacts (e.g., documents for development planning and software code). In particular, manufacturers will need to understand the principles of the new method, train their staff members, and maintain design and development records when creating the final product. The record will include design documents, meeting minutes, and other documents produced during the development. This effort causes a significant overhead in the time and work they have to invest before the product is ready for the market.[33]
Introducing quality management systems (QMS) by industry has proven to guarantee continuous high quality among projects and procedures within an organization. Our goal is to facilitate this experience in academic environments. Establishing an academia-tailored QMS for research organizations can address the described challenges of software quality, documentation, accessibility, traceability, and reproducibility and help software development in research organizations reach higher quality and standards. These quality standards are particularly critical for software that is intended to be used in the medical context. We can significantly reduce software transfer barriers among researchers in academia and industry if these standards are established from the start.
Moreover, it has the potential to facilitate and speed up the transfer to clinical practice and thereby improve medical diagnosis or treatment of patients rapidly. However, our recommendations are based on standards that are common for medical device development but do not have the intention to shortcut any steps of the regular medical device development; this will always have to be done according to the strict rules and regulations that apply. Other benefits of a QMS for medical device development are also beneficial for research organizations when developing such software, including making responsibilities clearer, phasing in new team members quickly, and ensuring everyone knows how their work contributes to project and organizational goals.
Requirements for QM are defined in ISO 9001[34], in ISO 13485[35], and the Code of Federal Regulation (CFR) Title 21.[36] However, while ISO 9001 is generic and can be used in different fields, ISO 13485 is specific for QM in medical device development. The main differences are that ISO 9001 requires the organization to demonstrate continual improvement. In contrast, ISO 13485 only requires the certified organization to verify that the QMS is effectively implemented and maintained. Additionally, ISO 9001 includes customer satisfaction, which is not relevant to ISO 13485. There are also some other differences in ISO 13485, e.g., that the promotion and awareness of regulatory requirements is a management responsibility, that risk assessment and management need to be carried out (according to ISO 14971), and some others. Unfortunately, ISO 13485 is most likely outside of what is feasible for research groups in universities and other research organizations.
Our goal: Academia-tailored QMS
Until now, there has been no guidance on how to establish an academia-tailored QMS for research organizations that balances between not having any QMS at all and a wholly formulated QMS that complies with official regulatory standards. Here, we present a synopsis of relevant requirements in such standards and adjust these toward software development requirements in academia. We aim to embrace the benefits and facilitate the technology transfer as much as possible while keeping the overhead for researchers and developers in a well manageable range. Thus, we tailor the content for use in universities or similar research organizations that focus on software in the medical setting.
However, the ideas presented here do not provide a shortcut when developing medical software. Any development of medical software must strictly follow the relevant regulations in the specific country or region. Therefore, our suggestions provide a starting point intended to be adapted to specific requirements as needed and we refer to it as MDx-ready (i.e., ready for transferring it into molecular diagnostics SaMD implementations). This flexibility is well in the mindset of most QMS: If there is a profound reason for the change, change it, but consider all relevant aspects and document the reasons and the changes.
QMS for medical software research
References
- ↑ Hawgood, Sam; Hook-Barnard, India G.; O’Brien, Theresa C.; Yamamoto, Keith R. (12 August 2015). "Precision medicine: Beyond the inflection point" (in en). Science Translational Medicine 7 (300): 300ps17–300ps17. doi:10.1126/scitranslmed.aaa9970. ISSN 1946-6234. https://stm.sciencemag.org/lookup/doi/10.1126/scitranslmed.aaa9970.
- ↑ Digital Health Center of Excellence (6 December 2017). "What are examples of Software as a Medical Device?". U.S. Food and Drug Administration. https://www.fda.gov/medical-devices/software-medical-device-samd/what-are-examples-software-medical-device.
- ↑ Fatima, Meherwar; Pasha, Maruf (2017). "Survey of Machine Learning Algorithms for Disease Diagnostic" (in en). Journal of Intelligent Learning Systems and Applications 09 (01): 1. doi:10.4236/jilsa.2017.91001. http://www.scirp.org/journal/PaperInformation.aspx?PaperID=73781&#abstract.
- ↑ 4.0 4.1 Batra, Richa; Alcaraz, Nicolas; Gitzhofer, Kevin; Pauling, Josch; Ditzel, Henrik J.; Hellmuth, Marc; Baumbach, Jan; List, Markus (1 December 2017). "On the performance of de novo pathway enrichment" (in en). npj Systems Biology and Applications 3 (1): 6. doi:10.1038/s41540-017-0007-2. ISSN 2056-7189. PMC PMC5445589. PMID 28649433. http://www.nature.com/articles/s41540-017-0007-2.
- ↑ 5.0 5.1 Hauschild, A.-C.; Baumbach, J.I.; Baumbach, J. (2012). "Integrated statistical learning of metabolic ion mobility spectrometry profiles for pulmonary disease identification". Genetics and Molecular Research 11 (3): 2733–2744. doi:10.4238/2012.July.10.17. http://www.funpecrp.com.br/gmr/year2012/vol11-3/pdf/gmr2065.pdf.
- ↑ 6.0 6.1 6.2 Jeanquartier, Fleur; Jean-Quartier, Claire; Kotlyar, Max; Tokar, Tomas; Hauschild, Anne-Christin; Jurisica, Igor; Holzinger, Andreas (2016), Holzinger, Andreas, ed., "Machine Learning for In Silico Modeling of Tumor Growth" (in en), Machine Learning for Health Informatics (Cham: Springer International Publishing) 9605: 415–434, doi:10.1007/978-3-319-50478-0_21, ISBN 978-3-319-50477-3, http://link.springer.com/10.1007/978-3-319-50478-0_21
- ↑ 7.0 7.1 Wiwie, Christian; Kuznetsova, Irina; Mostafa, Ahmed; Rauch, Alexander; Haakonsson, Anders; Barrio-Hernandez, Inigo; Blagoev, Blagoy; Mandrup, Susanne et al. (1 May 2019). "Time-Resolved Systems Medicine Reveals Viral Infection-Modulating Host Targets" (in en). Systems Medicine 2 (1): 1–9. doi:10.1089/sysm.2018.0013. ISSN 2573-3370. PMC PMC6524659. PMID 31119214. https://www.liebertpub.com/doi/10.1089/sysm.2018.0013.
- ↑ Calvert, Jacob; Saber, Nicholas; Hoffman, Jana; Das, Ritankar (13 February 2019). "Machine-Learning-Based Laboratory Developed Test for the Diagnosis of Sepsis in High-Risk Patients" (in en). Diagnostics 9 (1): 20. doi:10.3390/diagnostics9010020. ISSN 2075-4418. PMC PMC6468682. PMID 30781800. http://www.mdpi.com/2075-4418/9/1/20.
- ↑ Desautels, Thomas; Calvert, Jacob; Hoffman, Jana; Jay, Melissa; Kerem, Yaniv; Shieh, Lisa; Shimabukuro, David; Chettipally, Uli et al. (30 September 2016). "Prediction of Sepsis in the Intensive Care Unit With Minimal Electronic Health Record Data: A Machine Learning Approach" (in en). JMIR Medical Informatics 4 (3): e28. doi:10.2196/medinform.5909. ISSN 2291-9694. PMC PMC5065680. PMID 27694098. https://medinform.jmir.org/2016/3/e28/.
- ↑ Chen, Robert; Stewart, Walter F.; Sun, Jimeng; Ng, Kenney; Yan, Xiaowei (1 October 2019). "Recurrent Neural Networks for Early Detection of Heart Failure From Longitudinal Electronic Health Record Data: Implications for Temporal Modeling With Respect to Time Before Diagnosis, Data Density, Data Quantity, and Data Type" (in en). Circulation: Cardiovascular Quality and Outcomes 12 (10). doi:10.1161/CIRCOUTCOMES.118.005114. ISSN 1941-7713. PMC PMC6814386. PMID 31610714. https://www.ahajournals.org/doi/10.1161/CIRCOUTCOMES.118.005114.
- ↑ Heider, Dominik; Dybowski, Jan Nikolaj; Wilms, Christoph; Hoffmann, Daniel (1 December 2014). "A simple structure-based model for the prediction of HIV-1 co-receptor tropism" (in en). BioData Mining 7 (1): 14. doi:10.1186/1756-0381-7-14. ISSN 1756-0381. PMC PMC4124776. PMID 25120583. https://biodatamining.biomedcentral.com/articles/10.1186/1756-0381-7-14.
- ↑ Riemenschneider, Mona; Hummel, Thomas; Heider, Dominik (1 December 2016). "SHIVA - a web application for drug resistance and tropism testing in HIV" (in en). BMC Bioinformatics 17 (1): 314. doi:10.1186/s12859-016-1179-2. ISSN 1471-2105. PMC PMC4994198. PMID 27549230. http://bmcbioinformatics.biomedcentral.com/articles/10.1186/s12859-016-1179-2.
- ↑ 13.0 13.1 13.2 13.3 13.4 13.5 13.6 13.7 Brito, Jaqueline J; Li, Jun; Moore, Jason H; Greene, Casey S; Nogoy, Nicole A; Garmire, Lana X; Mangul, Serghei (1 June 2020). "Recommendations to enhance rigor and reproducibility in biomedical research" (in en). GigaScience 9 (6): giaa056. doi:10.1093/gigascience/giaa056. ISSN 2047-217X. PMC PMC7263079. PMID 32479592. https://academic.oup.com/gigascience/article/doi/10.1093/gigascience/giaa056/5849489.
- ↑ 14.0 14.1 Riemenschneider, Mona; Wienbeck, Joachim; Scherag, André; Heider, Dominik (1 June 2018). "Data Science for Molecular Diagnostics Applications: From Academia to Clinic to Industry" (in en). Systems Medicine 1 (1): 13–17. doi:10.1089/sysm.2018.0002. ISSN 2573-3370. http://www.liebertpub.com/doi/10.1089/sysm.2018.0002.
- ↑ Guellec, D.; van Pottelsberghe de la Potterie, B. (14 June 2000). "The Impact of Public R&D Expenditure on Business R&D" (in en). OECD Science, Technology and Industry Working Papers 2000/04. doi:10.1787/670385851815. https://www.oecd-ilibrary.org/science-and-technology/the-impact-of-public-r-d-expenditure-on-business-r-d_670385851815.
- ↑ 16.0 16.1 16.2 16.3 16.4 Mangul, Serghei; Mosqueiro, Thiago; Abdill, Richard J.; Duong, Dat; Mitchell, Keith; Sarwal, Varuni; Hill, Brian; Brito, Jaqueline et al. (20 June 2019). "Challenges and recommendations to improve the installability and archival stability of omics computational tools" (in en). PLOS Biology 17 (6): e3000333. doi:10.1371/journal.pbio.3000333. ISSN 1545-7885. PMC PMC6605654. PMID 31220077. https://dx.plos.org/10.1371/journal.pbio.3000333.
- ↑ 17.0 17.1 Mangul, Serghei; Martin, Lana S.; Eskin, Eleazar; Blekhman, Ran (1 December 2019). "Improving the usability and archival stability of bioinformatics software" (in en). Genome Biology 20 (1): 47, s13059–019–1649-8. doi:10.1186/s13059-019-1649-8. ISSN 1474-760X. PMC PMC6391762. PMID 30813962. https://genomebiology.biomedcentral.com/articles/10.1186/s13059-019-1649-8.
- ↑ 18.0 18.1 18.2 18.3 18.4 18.5 Lee, Graham; Bacon, Sebastian; Bush, Ian; Fortunato, Laura; Gavaghan, David; Lestang, Thibault; Morton, Caroline; Robinson, Martin et al. (1 February 2021). "Barely sufficient practices in scientific computing" (in en). Patterns 2 (2): 100206. doi:10.1016/j.patter.2021.100206. PMC PMC7892476. PMID 33659915. https://linkinghub.elsevier.com/retrieve/pii/S2666389921000167.
- ↑ Wilkinson, Mark D.; Dumontier, Michel; Aalbersberg, IJsbrand Jan; Appleton, Gabrielle; Axton, Myles; Baak, Arie; Blomberg, Niklas; Boiten, Jan-Willem et al. (1 December 2016). "The FAIR Guiding Principles for scientific data management and stewardship" (in en). Scientific Data 3 (1): 160018. doi:10.1038/sdata.2016.18. ISSN 2052-4463. PMC PMC4792175. PMID 26978244. http://www.nature.com/articles/sdata201618.
- ↑ 20.0 20.1 Pinto, Gustavo; Wiese, Igor; Dias, Luiz Felipe (1 March 2018). "How do scientists develop scientific software? An external replication". 2018 IEEE 25th International Conference on Software Analysis, Evolution and Reengineering (SANER) (Campobasso: IEEE): 582–591. doi:10.1109/SANER.2018.8330263. ISBN 978-1-5386-4969-5. http://ieeexplore.ieee.org/document/8330263/.
- ↑ Coiera, Enrico; Ammenwerth, Elske; Georgiou, Andrew; Magrabi, Farah (1 August 2018). "Does health informatics have a replication crisis?". Journal of the American Medical Informatics Association 25 (8): 963–968. doi:10.1093/jamia/ocy028. ISSN 1527-974X. PMC PMC6077781. PMID 29669066. https://doi.org/10.1093/jamia/ocy028.
- ↑ Shickel, Benjamin; Tighe, Patrick James; Bihorac, Azra; Rashidi, Parisa (1 September 2018). "Deep EHR: A Survey of Recent Advances in Deep Learning Techniques for Electronic Health Record (EHR) Analysis". IEEE Journal of Biomedical and Health Informatics 22 (5): 1589–1604. doi:10.1109/JBHI.2017.2767063. ISSN 2168-2194. PMC PMC6043423. PMID 29989977. https://ieeexplore.ieee.org/document/8086133/.
- ↑ Goecks, Jeremy; Jalili, Vahid; Heiser, Laura M.; Gray, Joe W. (1 April 2020). "How Machine Learning Will Transform Biomedicine" (in en). Cell 181 (1): 92–101. doi:10.1016/j.cell.2020.03.022. PMC PMC7141410. PMID 32243801. https://linkinghub.elsevier.com/retrieve/pii/S0092867420302841.
- ↑ Anwar, Syed Muhammad; Majid, Muhammad; Qayyum, Adnan; Awais, Muhammad; Alnowami, Majdi; Khan, Muhammad Khurram (1 November 2018). "Medical Image Analysis using Convolutional Neural Networks: A Review" (in en). Journal of Medical Systems 42 (11): 226. doi:10.1007/s10916-018-1088-1. ISSN 0148-5598. http://link.springer.com/10.1007/s10916-018-1088-1.
- ↑ Clough, Emily; Barrett, Tanya (2016), Mathé, Ewy; Davis, Sean, eds., "The Gene Expression Omnibus Database", Statistical Genomics (New York, NY: Springer New York) 1418: 93–110, doi:10.1007/978-1-4939-3578-9_5, ISBN 978-1-4939-3576-5, PMC PMC4944384, PMID 27008011, http://link.springer.com/10.1007/978-1-4939-3578-9_5
- ↑ Tomczak, Katarzyna; Czerwińska, Patrycja; Wiznerowicz, Maciej (2015). "The Cancer Genome Atlas (TCGA): An immeasurable source of knowledge". Współczesna Onkologia 1A: 68–77. doi:10.5114/wo.2014.47136. ISSN 1428-2526. PMC PMC4322527. PMID 25691825. http://www.termedia.pl/doi/10.5114/wo.2014.47136.
- ↑ Voigt, Paul; von dem Bussche, Axel (2017) (in en). The EU General Data Protection Regulation (GDPR). Cham: Springer International Publishing. doi:10.1007/978-3-319-57959-7. ISBN 978-3-319-57958-0. http://link.springer.com/10.1007/978-3-319-57959-7.
- ↑ Maak, Travis G.; Wylie, James D. (1 August 2016). "Medical Device Regulation: A Comparison of the United States and the European Union" (in en). Journal of the American Academy of Orthopaedic Surgeons 24 (8): 537–543. doi:10.5435/JAAOS-D-15-00403. ISSN 1067-151X. http://journals.lww.com/00124635-201608000-00004.
- ↑ World Health Organization, ed. (2011). Development of medical device policies. WHO medical device technical series. Geneva, Switzerland: World Health Organization. ISBN 978-92-4-150163-7.
- ↑ Schwaber, Ken; Beedle, Mike (2002). Agile software development with Scrum. Series in agile software development. Upper Saddle River, NJ: Prentice Hall. ISBN 978-0-13-067634-4.
- ↑ Anderson, David J. (2010). Kanban: Successful evolutionary change for your technology business. Sequim, Washington: Blue Hole Press. ISBN 978-0-9845214-0-1. OCLC 699604917. https://www.worldcat.org/title/mediawiki/oclc/699604917.
- ↑ Zamith, Manuel; Gonçalves, Gil (2018). "Towards an Agile Development Model for Certifiable Medical Device Software - Taking Advantage of the Medical Device Regulation:". Proceedings of the 13th International Conference on Software Technologies (Porto, Portugal: SCITEPRESS - Science and Technology Publications): 132–140. doi:10.5220/0006861301320140. ISBN 978-989-758-320-9. http://www.scitepress.org/DigitalLibrary/Link.aspx?doi=10.5220/0006861301320140.
- ↑ Sharma, Arjun; Blank, Anthony; Patel, Parashar; Stein, Kenneth (1 March 2013). "Health care policy and regulatory implications on medical device innovations: A cardiac rhythm medical device industry perspective" (in en). Journal of Interventional Cardiac Electrophysiology 36 (2): 107–117. doi:10.1007/s10840-013-9781-y. ISSN 1383-875X. PMC PMC3606523. PMID 23474980. http://link.springer.com/10.1007/s10840-013-9781-y.
- ↑ "ISO 9001:2015 Quality management systems — Requirements". International Organization for Standardization. September 2015. https://www.iso.org/standard/62085.html.
- ↑ [https://www.iso.org/standard/59752.html "ISO 13485:2016 Medical devices — Quality management systems — Requirements for regulatory purposes"]. International Organization for Standardization. March 2016. https://www.iso.org/standard/59752.html.
- ↑ "CFR - Code of Federal Regulations Title 21". U.S. Food and Drug Administration. 1 April 2020. https://www.accessdata.fda.gov/scripts/cdrh/cfdocs/cfcfr/cfrsearch.cfm.
Notes
This presentation is faithful to the original, with only a few minor changes to presentation, though grammar and word usage was substantially updated for improved readability. In some cases important information was missing from the references, and that information was added. The original article lists references alphabetically, but this version—by design—lists them in order of appearance.