Journal:Users’ perspectives on a picture archiving and communication system (PACS): An in-depth study in a teaching hospital in Kuwait
| Full article title | Users’ perspectives on a picture archiving and communication system (PACS): An in-depth study in a teaching hospital in Kuwait |
|---|---|
| Journal | JMIR Medical Informatics |
| Author(s) | Buabbas, Ali Jassem; Al-Shamali, Dawood Ameer; Sharma, Prem; Haidar, Salwa; Al-Shawaf, Hamza |
| Author affiliation(s) | Kuwait University, Mubarak AlKabeer Hospital |
| Primary contact | Email: ali.buabbas [at] hsc.edu.kw; Phone: 965 25319504 |
| Editors | Eysenbach, G. |
| Year published | 2016 |
| Volume and issue | 4 (2) |
| Page(s) | e21 |
| DOI | 10.2196/medinform.5703 |
| ISSN | 2291-9694 |
| Distribution license | Creative Commons Attribution 2.0 |
| Website | http://medinform.jmir.org/2016/2/e21/ |
| Download | http://medinform.jmir.org/2016/2/e21/pdf (PDF) |
|
|
This article should not be considered complete until this message box has been removed. This is a work in progress. |
Abstract
Background: The picture archiving and communication system (PACS) is a well-known imaging informatics application in health care organizations, specifically designed for the radiology department. Health care providers have exhibited willingness toward evaluating PACS in hospitals to ascertain the critical success and failure of the technology, considering that evaluation is a basic requirement.
Objective: This study aimed to evaluate the success of a PACS in a regional teaching hospital of Kuwait, from users’ perspectives, using information systems success criteria.
Methods: An in-depth study was conducted by using quantitative and qualitative methods. This mixed-method study was based on: (1) questionnaires, distributed to all radiologists and technologists and (2) interviews, conducted with PACS administrators.
Results: In all, 60 questionnaires were received from the respondents. These included 39 radiologists (75% response rate) and 21 technologists (62% response rate), with the results showing almost three-quarters (74%, 44 of 59) of the respondents rating PACS positively and as user-friendly. This study’s findings revealed that the demographic data, including computer experience, was an insignificant factor, having no influence on the users’ responses. The findings were further substantiated by the administrators’ interview responses, which supported the benefits of PACS, indicating the need for developing a unified policy aimed at streamlining and improving the departmental workflow.
Conclusions: The PACS had a positive and productive impact on the radiologists’ and technologists’ work performance. They were endeavoring to resolve current problems while keeping abreast of advances in PACS technology, including teleradiology and the mobile image viewer, which is steadily increasing in usage in the Kuwaiti health system.
Keywords: PACS evaluation, user perspective, IS success, imaging informatics, radiology
Introduction
The picture archiving and communication system (PACS) is a well-known imaging informatics application in health care organizations, specifically designed for the radiology department. A PACS could be defined as “an electronic information system (IS) used to acquire, store, transmit, and display medical images.”[1] Using a PACS in a hospital has innumerable benefits at various levels.[2] At the management level, this technology has direct implications for cost reduction, rendering the film production process redundant. At the departmental level, the technology enhances productivity, as all tasks are performed digitally and swiftly. And at the clinical level, image interpretation and diagnosis become more precise and accurate.[3] For these reasons, health care organizations are increasingly adopting the PACS in their clinical radiology departments, despite the high costs, to benefit from the full advantages of using the technology. PACSs are currently being applied in many medical imaging projects around the world, such as in the United States, the United Kingdom, and Asia. However, the available literature reveals gaps with regard to the systems’ effectiveness and efficiency concerning their intended use.
The existing literature abounds with studies evaluating the PACS.[4] However, these evaluations invariably had different focuses and objectives; for instance, there are studies on the PACS before and after the system’s implementation[5], users’ satisfaction[6], PACS acceptance[7], cost-effectiveness[8][9], and the system’s efficiency concerning its use and in saving time.[10] The most widely used form of the PACS evaluation concerns its impact on users.[4][11][12]
In PACS research and practice, once the system has been adopted and implemented, it becomes imperative to evaluate the technology’s effectiveness within an organization.[13] For all practical purposes, evaluation could be defined as “the process of describing the implementation of an information resource and judging its merits and worth.”[14] IS deployment may invariably lead to unintended consequences, affecting the chances of the technology’s success.[14] Several researchers have, therefore, recommended evaluation studies specially focused on PACSs to assess their impact in clinical practice [4,15].[4][15]
It is of paramount significance to investigate the success of the PACS, exploring the factors responsible for the success or failure to determine its worth clinically, based on the direct users of this system.
The conceptual basis of this study is focused on this: the impact of a PACS in a regional hospital in Kuwait based on specific criteria. This study is the first of its kind in Kuwait, there being a scarcity of literature in this field.
Research questions
The research questions were specifically as follows: (1) What impact does the PACS have on the clinical practice of radiologists and technologists in the radiology department of Mubarak Al-Kabeer Hospital? (2) Has the use of the PACS proven successful in improving the radiology department’s work performance?
This study aimed at evaluating the success of the PACS in clinical practice, in a bid to determine the technology’s merits for radiologists and technologists, including its drawbacks.
Methods
Research settings
The universe of this study was Mubarak Al-Kabeer Teaching Hospital, which is one of the five regional hospitals in the State of Kuwait. Table 1 presents the site’s profile.
| ||||||||||||||||||
This general hospital is a university-teaching hospital in Kuwait and was chosen because it is always at the forefront of development and advanced medicine. Therefore, to ensure the full advantage of the health information system (HIS), the PACS’s success needed to be verified. The PACS was first introduced in the radiology department of Mubarak Al-Kabeer Hospital in 2004, marking the transition of clinical services from a film-based system to an electronic-based system. The PACS used is an off-the-shelf, Oracle-based HIS (GE Centrisity RIS i 4.2 plus, GE PACS IW 3.7.3.9 SP 3). The PACS currently has 35 workstations, with a server capacity of 64 terabytes. Radiologists use the PACS to view images through the radiology information system (RIS), which they use to report their cases. The reports generated by the RIS are then sent to the PACS, through which final reports can be sent to the HIS. The treating physician needs to submit an access request to see patients’ images on the PACS. In June 2013, the PACS software was upgraded, and currently the system is fully integrated technically with the RIS and the HIS, providing the users with a secure system.
Study design
An in-depth study was conducted by using quantitative and qualitative methods. This mixed-method study was based on: (1) survey questionnaires, which were distributed to gather information from radiologists and technologists in the radiology department of Mubarak Al-Kabeer Hospital and (2) semi structured interviews, which were conducted to gather empirical information from the PACS administrators. Ethical approval for the study was obtained from the research department of the Ministry of Health, Kuwait.
To gather the responses of radiologists and technologists concerning the use of the PACS in their clinical practice, a validated questionnaire from a previous study was used.[16] The questionnaire was translated from French into English through an official translation office in Kuwait. The English version of the questionnaire was pretested with five radiologists and three technologists to ensure the suitability and usability of the questions. Accordingly, a number of amendments were made to the questionnaire. These included excluding questions that were found to be irrelevant to the technologists’ use of the PACS, which comprised items that focused on retrieving, displaying, comparing, and manipulating images, including confidence level. In addition, a seven-point Likert scale was changed to five points to make it easier and more familiar for the respondents.
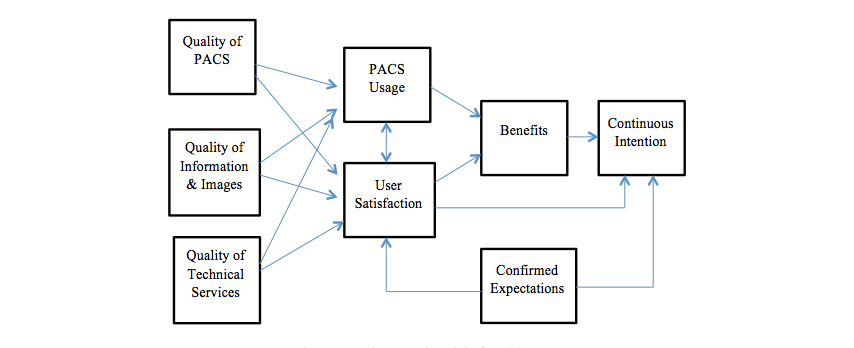
In this study, evaluating the PACS’s success was based on an integrated multidimensional model, which was constructed from the model primarily developed by DeLone and McLean[17][18], later developed with two constructs added to the model, namely system continuance intention and confirmation of expectations.[16] (See Figure 1.)
|
The questionnaire comprised seven sections (Textbox 1) for assessing the users’ perspectives on eight interrelated dimensions of the PACS success model. These included: (1) perceived system quality; (2) perceived information quality; (3) perceived service quality; (4) system usage; (5) user satisfaction; (6) perceived net benefits; (7) system continuance intention; and (8) confirmed expectations. The questionnaire was distributed to all radiologists and radiology technologists who had used the PACS in their clinical practice for the last two years.
|
The data gathered through the questionnaire were complemented by conducting semi-structured interviews with PACS administrators to gain an understanding of the prevailing clinical environment, which entails them communicating with radiologists, doctors, and technologists, including providing information technology services and support.[19] Their experience further enriched the information gathered and the study’s purpose.
The focus of the interviews was primarily similar to that of the questionnaire: to gain a deeper insight into the response patterns of the respondents. The interviews were conducted with the radiology technologists, who are responsible for administering the PACS and overseeing the RIS operations in the radiology department.
Statistical analysis
Data management, analysis, and graphical presentation were carried out using the software Statistical Package for the Social Sciences (SPSS), version 22.0. The questionnaire was evaluated for internal consistency and reliability, and Cronbach alpha values were estimated for major perspectives by combining the Likert scale items for specific aspects, including quality, information, images, technical support and usage, user satisfaction, and overall opinion on the PACS. The descriptive statistics analysis generated frequencies and percentages for all the five-point Likert scale items (1 as lowest or strongly disagree and 5 as highest or strongly agree) in the questionnaire. The Likert scale data were also analyzed to find average values for overall responses and to compare the mean (±standard deviation, SD) between radiologists and technologists using t tests or nonparametric Mann-Whitney tests. The quantitative or continuous variables, age, duration of use (h), and minutes saved every day were first ascertained for normal distribution, applying the Kolmogorov-Smirnov test and were presented as mean ± SD and range for normally distributed variables and as median, range and interquartile (IQ) for skewed data. The chi-square or Fisher exact test was applied to find any association or significant difference between categorical variables. The Spearman correlation coefficient (rho) was used to find any correlations among the number of hours worked, the use of the PACS, and the minutes saved in daily practice. The two-tailed probability value P<.05 was considered statistically significant.
Results
References
- ↑ Tzeng, W.S.; Kuo, K.M.; Lin, H.W.; Chen, T.Y. (2013). "A socio-technical assessment of the success of Picture Archiving and Communication Systems: The radiology technologist's perspective". BMC Medical Informatics and Decision Making 13: 109. doi:10.1186/1472-6947-13-109. PMC PMC3849362. PMID 24053458. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3849362.
- ↑ Vest, J.R.; Jung, H.Y.; Ostrovsky, A. et al. (2015). "Image Sharing Technologies and Reduction of Imaging Utilization: A Systematic Review and Meta-analysis". Journal of the American College of Radiology 12 (12 Pt B): 1371-1379.e3. doi:10.1016/j.jacr.2015.09.014. PMC PMC4730956. PMID 26614882. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4730956.
- ↑ Duyck, P.; Pynoo, B.; Devolder, P. et al. (2010). "Monitoring the PACS implementation process in a large university hospital: Discrepancies between radiologists and physicians". Journal of Digital Imaging 23 (1): 73–80. doi:10.1007/s10278-008-9163-7. PMC PMC3043749. PMID 18956231. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3043749.
- ↑ 4.0 4.1 4.2 Hains, I.M.; Georgiou, A.; Westbrook, J.I. (2012). "The impact of PACS on clinician work practices in the intensive care unit: a systematic review of the literature". JAMIA 19 (4): 506–13. doi:10.1136/amiajnl-2011-000422. PMC PMC3384105. PMID 22323392. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3384105.
- ↑ Bryan, S.; Weatherburn, G.C.; Watkins, J.R.; Buxton, M.J. (1999). "The benefits of hospital-wide picture archiving and communication systems: A survey of clinical users of radiology services". The British Journal of Radiology 72 (857): 469-78. doi:10.1259/bjr.72.857.10505012. PMID 10505012.
- ↑ Tan, S.L.; Lewis, R.A. (2010). "Picture archiving and communication systems: A multicentre survey of users experience and satisfaction". European Journal of Radiology 75 (3): 406–10. doi:10.1016/j.ejrad.2009.05.008. PMID 19523778.
- ↑ Aldosari, B. (2012). "User acceptance of a picture archiving and communication system (PACS) in a Saudi Arabian hospital radiology department". BMC Medical Informatics and Decision Making 12: 44. doi:10.1186/1472-6947-12-44. PMC PMC3423046. PMID 22640490. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3423046.
- ↑ Bryan, S.; Weatherburn, G.; Buxton, M. et al. (1999). "Evaluation of a hospital picture archiving and communication system". Journal of Health Services Research and Policy 4 (4): 204-9. doi:10.1177/135581969900400405. PMID 10623035.
- ↑ Moodley, I.; Moodley, S. (2015). "A comparative cost analysis of picture archiving and communications systems (PACS) versus conventional radiology in the private sector". South African Journal of Radiology 19 (1): 634-641. doi:10.4102/sajr.v19i1.634.
- ↑ Mackinnon, A.D.; Billington, R.A.; Adam, E.J. et al. (2008). "Picture archiving and communication systems lead to sustained improvements in reporting times and productivity: Results of a 5-year audit". Clinical Radiology 63 (7): 796-804. doi:10.1016/j.crad.2007.12.015. PMID 18555038.
- ↑ van de Wetering, R.; Batenburg, R.; Versendaal, J. et al. (2006). "A balanced evaluation perspective: Picture archiving and communication system impacts on hospital workflow". Journal of Digital Imaging 19 (Suppl 1): 10. doi:10.1007/s10278-006-0628-2. PMC PMC3045172. PMID 16763932. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3045172.
- ↑ Creswick, N.; Hains, I.M.; Westbrook, J.I. (2011). "Innovation in intensive care nursing work practices with PACS". Studies in Health Technology and Informatics 169: 402–6. doi:10.3233/978-1-60750-806-9-402. PMID 21893781.
- ↑ van de Wetering, R.; Batenburg, R. (2014). "Towards a theory of PACS deployment: An integrative PACS maturity framework". Journal of Digital Imaging 27 (3): 337–50. doi:10.1007/s10278-013-9671-y. PMC PMC4026462. PMID 24448919. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4026462.
- ↑ 14.0 14.1 Friedman, C.P.; Wyatt, J. (2006). Evaluation Methods in Biomedical Informatics. Springer-Verlag New York. pp. 386. doi:10.1007/0-387-30677-3. ISBN 9780387258898.
- ↑ Mansoori, B.; Erhard, K.K.; Sunshine, J.L. (2012). "Picture Archiving and Communication System (PACS) implementation, integration & benefits in an integrated health system". Academic Radiology 19 (2): 229–35. doi:10.1016/j.acra.2011.11.009. PMID 22212425.
- ↑ 16.0 16.1 Paré, G.; Lepanto, L.; Aubry, D.; Sicotte, C. (2005). "Toward a multidimensional assessment of picture archiving and communication system success". International Journal of Technology Assessment in Health Care 21 (4): 471–9. doi:10.1017/S0266462305050658. PMID 16262970.
- ↑ DeLone, W.H.; McLean, E.R. (1992). "Information Systems Success: The Quest for the Dependent Variable". Information Systems Research 3 (1): 60–95. doi:10.1287/isre.3.1.60.
- ↑ DeLone, W.H.; McLean, E.R. (2003). "The DeLone and McLean Model of Information Systems Success: A Ten-Year Update". Journal of Management Information Systems 19 (4): 9–30. doi:10.1080/07421222.2003.11045748.
- ↑ Joshi, V.; Narra, V.R.; Joshi, K. (2014). "PACS administrators' and radiologists' perspective on the importance of features for PACS selection". Journal of Digital Imaging 27 (4): 486-95. doi:10.1007/s10278-014-9682-3. PMC PMC4090402. PMID 24744278. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4090402.
Abbreviations
CAD: computer-assisted diagnosis
HIS: health information system
ID: identification
IS: information system
PACS: picture archiving and communication System
RIS: radiology information system
Notes
This presentation is faithful to the original, with only a few minor changes to presentation. In several cases the PubMed ID was missing and was added to make the reference more useful.
Per the distribution agreement, the following copyright information is also being added:
©Ali Jassem Buabbas, Dawood Ameer Al-Shamali, Prem Sharma, Salwa Haidar, Hamza Al-Shawaf. Originally published in JMIR Medical Informatics (http://medinform.jmir.org), 15.06.2016.