Journal:Implement an international interoperable PHR by FHIR: A Taiwan innovative application
| Full article title | Implement an international interoperable PHR by FHIR: A Taiwan innovative application |
|---|---|
| Journal | Sustainability |
| Author(s) | Lee, Yen-Liang; Lee, Hsiu-An; Hsu, Chien-Yeh; Kung, Hsin-Yeh; Chiu, Hung-Wen |
| Author affiliation(s) |
Taipei Medical University, Chunghwa Telecom Laboratories, Tamkang University, Smart Healthcare Center of Excellence, National Taipei University of Nursing and Health Sciences |
| Primary contact | hwchiu at tmu dot edu dot tw |
| Year published | 2020 |
| Volume and issue | 13(1) |
| Article # | 198 |
| DOI | 10.3390/su13010198 |
| ISSN | 2071-1050 |
| Distribution license | Creative Commons Attribution 4.0 International |
| Website | https://www.mdpi.com/2071-1050/13/1/198/htm |
| Download | https://www.mdpi.com/2071-1050/13/1/198/pdf (PDF) |
Abstract
Personal health records (PHRs) have many benefits for things such as health surveillance, epidemiological surveillance, self-control, links to various services, public health and health management, and international surveillance. The implementation of an international standard for interoperability is essential to accessing PHRs. In Taiwan, the nationwide exchange platform for electronic medical records (EMRs) has been in use for many years. The Health Level Seven International (HL7) Clinical Document Architecture (CDA) was used as the standard for those EMRs. However, the complication of implementing CDA became a barrier for many hospitals to realizing standard EMRs.
In this study, we implemented a Fast Healthcare Interoperability Resources (FHIR)-based PHR transformation process, including a user interface module to review the contents of PHRs. We used My Health Bank (MHB), a PHR data book developed and issued to all people by the Taiwan National Health Insurance, as the PHRs' contents in this study. Network Time Protocol (NTP)/Simple Network Time Protocol (SNTP) was used in the security and user authentication mechanism when processing and applying personal health information. Transport Layer Security (TLS) 1.2 (such as HyperText Transfer Protocol Secure or HTTPS) was used for protection in data communication. User authentication is important in the platform. OAuth (OAuth 2.0) was used as a user authentication mechanism to confirm legitimate user access to ensure data security. The contents of MHB were analyzed and mapped to FHIR, and then converted to FHIR format according to the mapping logic template. The function of format conversion was carried out by using ASP.NET. XPath and JSPath technologies filtered out specific information tags. The converted data structure was verified through an HL7 application programming interface (HAPI) server, and a new JSON file was finally created.
This platform can not only capture any PHR based on the FHIR format but also publish FHIR-based MHB records to any other platform to bridge the interoperability gap between different PHR systems. Therefore, our implementation/application with the automatic transformation from MHB to FHIR format provides an innovative method for people to access their own PHRs through MHB. No one has published a similar application like us using a nationwide PHR standard, MHB, in Taiwan. The application we developed will be very useful for a single person to use or for other system developers to implement their own standard PHR software.
Keywords: FHIR, interoperability, PHR, data management, precision health management
Introduction
Personal health records (PHRs) are personalized records that include data related to health.[1] The Markle Foundation’s "Connecting for Health" collaborative defines a PHR as “an electronic application through which individuals can access, manage, and share their health information, and that of others for whom they are authorized, in a private, secure, and confidential environment.”[2] This differs from the more widely used electronic medical record (EMR), which focuses on clinical data and is operated by the medical service provider (such as clinics and hospitals). PHRs have great benefits for health monitoring, epidemiological surveillance, self-control, linkages with different services, and public health management in areas such as international health care.[3][4]
Recently, medical services have placed more focus on precision medicine, which refers to specific medical treatments based on the individual characteristics of each patient.[5] PHRs are a crucial component of precision medicine. The information in PHRs can provide more details for clinical decision support. Based on a foundation of an electronic hospital information system (HIS), we can get plentiful personal health data to create PHRs. Taiwan has implemented national centralized health insurance information systems since the establishment of the Taiwan National Health Insurance Administration (NHIA) in 1995. According to CEOWORLD magazine’s 2019 “Health Care Index” statistics, Taiwan has the best medical system in the world[6], while the National Health Insurance (NHI) has a coverage rate of more than 99%.[7] The NHIA pays for most of the medical service expenses of all Taiwanese citizens to the hospitals and clinics that provide services. For the reimbursement procedure, hospitals and clinics need to upload patient care data related to the payment, including the diagnosis, prescriptions, treatment information, images, testing data, etc. to NHIA information systems. By doing so, the NHIA has collected almost all individual medical care data in Taiwan and stores it at the NHIA’s data center. To promote personal health management, the NHIA launched the My Health Bank (MHB) system in September 2014. The MHB system is a personalized cloud-based service that aims to return personal medical data back to the citizens. Individuals can use their citizen digital certificate or password-registered NHI card as identity verification to download their medical data that have been collected by health insurance.
The NHIA aims to let citizens more directly control and manage their health data. Based on a cloud-based system, people can access their personal health insurance records in the past three years via the NHIA’s MHB portal, and the data can be printed out or downloaded. The NHIA hopes that citizens will have access to MHB when they go to a clinic or hospital as a reference for the physician. This service promotes people to have their health information and know their own health status.
However, despite the rich content of MHB and the data quality of the information confirmed in diagnosis, medicine, and other items, the information continues to use the original insurance declaration form and does not follow the relevant medical information standards. This makes it difficult to integrate and apply information. In addition, the official MHB system is mainly used as a data provider. The content is mainly based on the qualified medical insurance service records of various contracted hospitals, clinics, or institutions. Individuals are not allowed to add other personalized information themselves. Additionally, cloud-based systems can make it hard to share data with the doctor. When people see a doctor for an urgent reason, there may not be enough time to log into the MHB system and search for data. Although individuals can download data from the website, the data will be in the XML or JSON format, which most individuals cannot read. In addition, the content of PHRs does not follow any international format, making it quite difficult to exchange data or interoperate with other health information systems. The application and sharing of PHRs are very important. In order to achieve precision medicine, PHRs need to comply with international standards before they can be accepted, integrated, and applied by different systems.
Jung et al.[8] agree that an integrated personal health record is more valuable than a single record. The impact of interoperability on PHRs has been the focus of interdisciplinary researchers in recent years. A survey article by Alyami and Song[9] emphasized the vital role of interoperability in the implementation and adoption of PHRs. Plastiras and O'Sullivan[10] developed an ontology-driven intermediary layer to achieve interoperability between PHRs and electronic health records (EHRs) of various standards. Li[11] developed a service-oriented interoperable integrated PHR system and explained that it can be used to overcome interoperability problems between medical systems. Urbauer et al.[12] compared the interoperability procedures for the communication of medical systems and personal health devices to analyze the advantages and gaps, including presenting a total solution for interoperability. And Roehrs et al.[13] presented the crucial concept of interoperability for developing and using PHRs.
According to other related studies, the key point of PHR applications from different sources is application integration and content standardization. In general, currently, most of the interoperability of medical information is still based on standardized data exchange and integration through the development of intermediary layers, data standard conversion, or ontology design. Taiwan has an advanced health insurance system and has collected complete personal health records since 1995. The huge health database gives Taiwan a good opportunity for precision medicine to use. However, due to the delayed process of government authority on the implementation of the data standardization and formatting, the data still cannot meet the requirements of international interoperability at present.
In Taiwan, the nationwide exchange platform for EMRs has been in use for many years. Although the Health Level Seven International (HL7) CDA was used as the standard of the EMRs, people outside the hospitals, including patients and many health management organizations, did not have the method to access the EMRs, and the complication of implementing CDA became a barrier for hospitals to realize the standard EMRs. As such, a concept was developed: the implementation with an automatic transformation from MHB to a Fast Healthcare Interoperability Resources (FHIR) format provides an innovative method for people to access their own PHRs through MHB. No one has published a similar application like us to use nationwide PHRs, i.e., MHB, in Taiwan. The application we developed will be very useful for a single person to use or for other system developers to implement their own standard PHR software.
This research focuses on converting Taiwan’s personal health information into a standardized international standard format and provide a management platform for personal health records. Based on an innovative application model of personal data (MHB) unique to Taiwan’s health insurance, we designed a demonstration framework to enable Taiwan to have better exemplary measures in personal health management, and take the lead in completing “patient-centered” precise health management. The goal of this study was to develop an interoperable international personal health record using HL7 FHIR as the data standard and MHB data as the data content. This study designed a personal health management platform that could fit international standards and support users to manage personal health based on MHB. As long as the FHIR format health record is uploaded, people from different countries can use it all over the world to manage their personal health information, allow physicians to conduct precise medical treatment, and provide clinical decision-making support to users.
Literature review
Personal health information is an important foundation for the development of smart medical care. In addition to EMRs for medical consultations, institutional care records, and physiological data measured by medical materials, it also includes daily food content and wound conditions, which can be included in personal health records.
Although there are many standards in the medical domain, the interoperability between different systems is still poor. There are many problems that need to be solved for system interoperability. Therefore, HL7 has developed FHIR as a new foundation to achieve interoperability. FHIR is currently a widely adopted health information standard. It is not a kind of EHR; rather, it describes the data format and data elements of EHRs. FHIR is the new HL7 standard that evolved from the HL7 v2, HL7 v3, and HL7 CDA standards, which aim for easier implementation.[14] The main goals of FHIR are to promote the effective communication and content of medical information and to widely use medical information on a variety of devices, including computers, tablets, IoT devices, and smartphones, so as to provide medical services to hospitals and individuals more easily. It also provides systematic information to third-party application developers. FHIR has the characteristics and value of being open and easy to expand by publicly providing data elements in a standardized format. It also provides an alternative to document-centric approaches by providing different data elements separately as a service. For example, with the corresponding resource URLs, basic healthcare service elements such as patients, admissions, diagnostic reports, and medications can be accessed and manipulated. The implementation of FHIR is based on the HL7 and HTTPS (HTTP Secure) protocols; therefore, the wire data analysis platform can parse messages for real-time data collection. According to this idea, when FHIR messages are transmitted over the network, the medical service organization will be able to use these messages to collect real-time data. This data can then be fed into the data store where it is associated with other informatics data. FHIR uses a web-based API suite, including HTML, HTTP-based RESTful protocols, and cascading style sheets (CSS) for the user interface. The document format can be based on the JSON or XML format.
Schleyer et al. created a medical dashboard based on FHIR that integrates clinical information from the HISs with the EHR. Testing in a medical organization showed that the integration dashboard is useful. The clinical information can be integrated effectively based on FHIR.[15] FHIR uses widely adopted web technologies, is implementer-friendly and vendor-independent, and offers a useful architecture of applications and formats for EHR providers, healthcare providers, and public health professionals.[16] Baihan et al. implemented FHIR in the m-Health domain and used FHIR to integrate health information technology (HIT) systems with m-Health applications.[17] Daumke presented an architecture to harmonize commercial clinical text-mining tools by FHIR, which can be used as a clinical information model standard.[18] Recently, many research and industry products provide examples of how FHIR can be used for healthcare data integration [19][20][21][22][23][24][25][26], highlighting how FHIR has realized interoperability between different healthcare systems.
However, Taiwan’s MHB is not designed with reference to the good examples of other studies. Many adjustments are needed in terms of data compatibility, interoperability, and standardization.
Roehrs et al.[27] proposed an application model to buffer the integration problems caused by the lack of interoperability between different standards. Medical organizations have also proposed various standards to alleviate interoperability problems, and convert some of the more popular standards into Unified Modeling Language (UML) to achieve model-driven development of medical and health applications.[28][29] González-Ferrer et al.[30] developed a PHR-based clinical decision support system, making PHR a core component of clinical decision support (CDS). After evaluation, the implementation was completed using openEHR and HL7 virtual medical records (vMRs). Simon et al. developed Ubiquitous PHR (uPHR)[31], which emphasizes data interoperability standards across different healthcare institutions. Marceglia et al.[32] designed a structured mobile PHR application. The application allows the use of HL7 CDA and an EHR (OpenEMR) for cloud sharing of health records to exchange information. Fonda et al.[33] developed a prototype personal health application (PHA) for patient-centered diabetes self-management. Under the Project Health Design program, a study[34] used “Observation of Daily Life” (ODL) to monitor personal health, such as PHRs for elderly people with arthritis and PHRs for self-assessment of asthma patients. Ferguson et al.[35] designed a personal health application for patients with heart failure. And Siek et al. developed the “Colorado Nursing Tablet”[36] to help the elderly and their visiting caregivers manage medication plans during care.
According to other integrated information technology architecture research, the interoperability of health data and data integration are the key points of development, which can effectively improve the availability of information systems and medical data, and provide convenient operating tools through an incapable architecture. Even though other studies have proposed prototypes of application systems, they still have some weaknesses. First, most systems are aimed at patients with specific diseases, such as Alzheimer’s, heart disease, diabetes, etc., which reduces the interoperability and data integration. Second, the data are still based on specific disease groups and data content, and there is still a gap in follow-up treatment tracking and health management. Third, the patient’s ability to manage and track data still needs to be strengthened.
Materials and methods
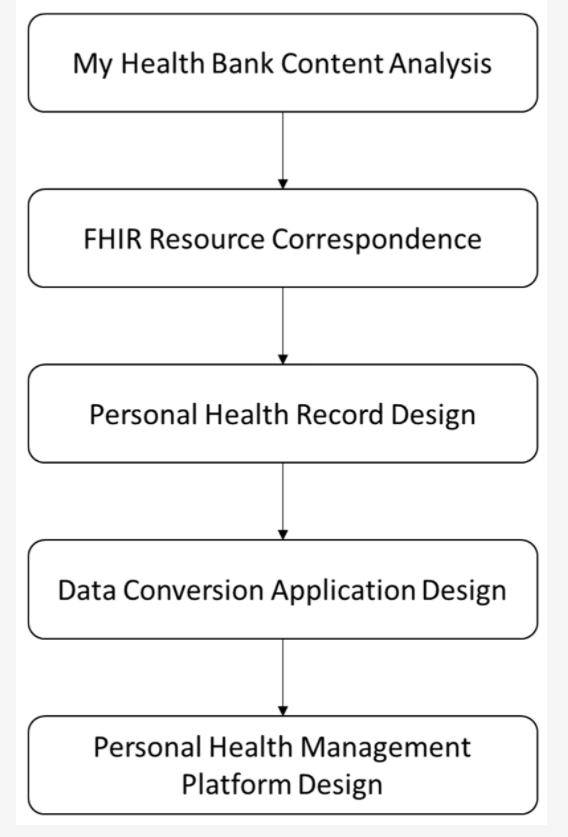
This research designed an FHIR-based personal health record adapter based on My Health Bank provided by the NHIA. Finally, an FHIR-compliant personal health management platform was established as a demonstration case. The research process of this research is shown in Figure 1.
|
My Health Bank (MHB) content analysis
MHB was launched by the NHIA in 2014. MHB is a personalized cloud-based service that aims to return personal medical data back to citizens. People can access their personal records and preventive health information from anywhere, and MHB data can be printed out or downloaded. However, the MHB system does not allow individuals to add other personalized information. The content is only claim-based medical data related to the National Health Insurance reimbursement process. Moreover, MHB does not comply with international standards. Although it is possible to get the data from the website, individuals still cannot read it themselves or exchange it with other organizations.
MHB data includes the data owner’s basic data and 11 other categories of data: outpatient data, inpatient data, dental data, allergy data, organ donation or palliative and hospice medical care choice, immunization information data, laboratory test data, imaging or pathological examination reports, traditional Chinese medicine data, and adult preventive data. The MHB data items are shown in Table 1. Different items have different content.
| ||||||||||||||||||||||||||
The content of the personal basic data includes national ID and name. Outpatient data, inpatient data, dental data, and traditional Chinese medicine data refer to clinical information and contain their own categories: medical institution details, medical date, disease diagnosis, personal payment amount, health insurance payment points, and prescription details. Allergy data can support physicians when prescribing medicine. Organ donation and palliative and hospice medical care choice data are part of MHB data, which the data owner decides in advance. When there is a note in this section, the patient’s hospice medical behavior will be decided accordingly. The content of preventive inoculation data includes vaccination data, vaccination dates, and medical institution details. The content of laboratory test, imaging, or pathological examination reports, and screening data, which can improve medical service efficiency and reduce medical provider burden, include laboratory testing item or order details, result value, reference value, medical institution details, and image or pathology reports. Adult preventive data refer to preventive care and include height, weight, body mass index, waist circumference, blood pressure, cholesterol, blood sugar, kidney function, urine routine, metabolic syndrome, liver function, hepatitis B status, and hepatitis C status.
Different items have different data presentation methods and structures. The MHB is converted to the FHIR format after comparing the code of the MHB with the PHR items.
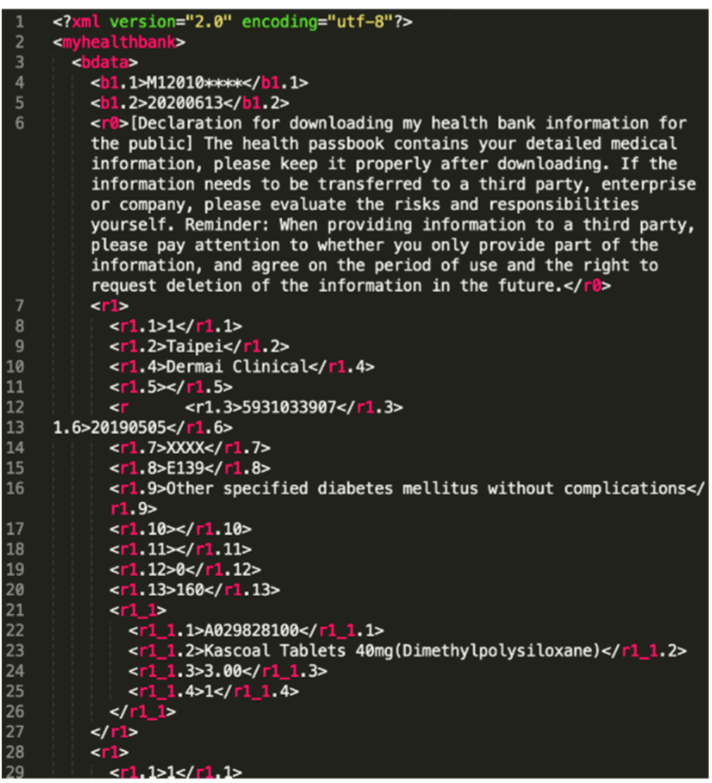
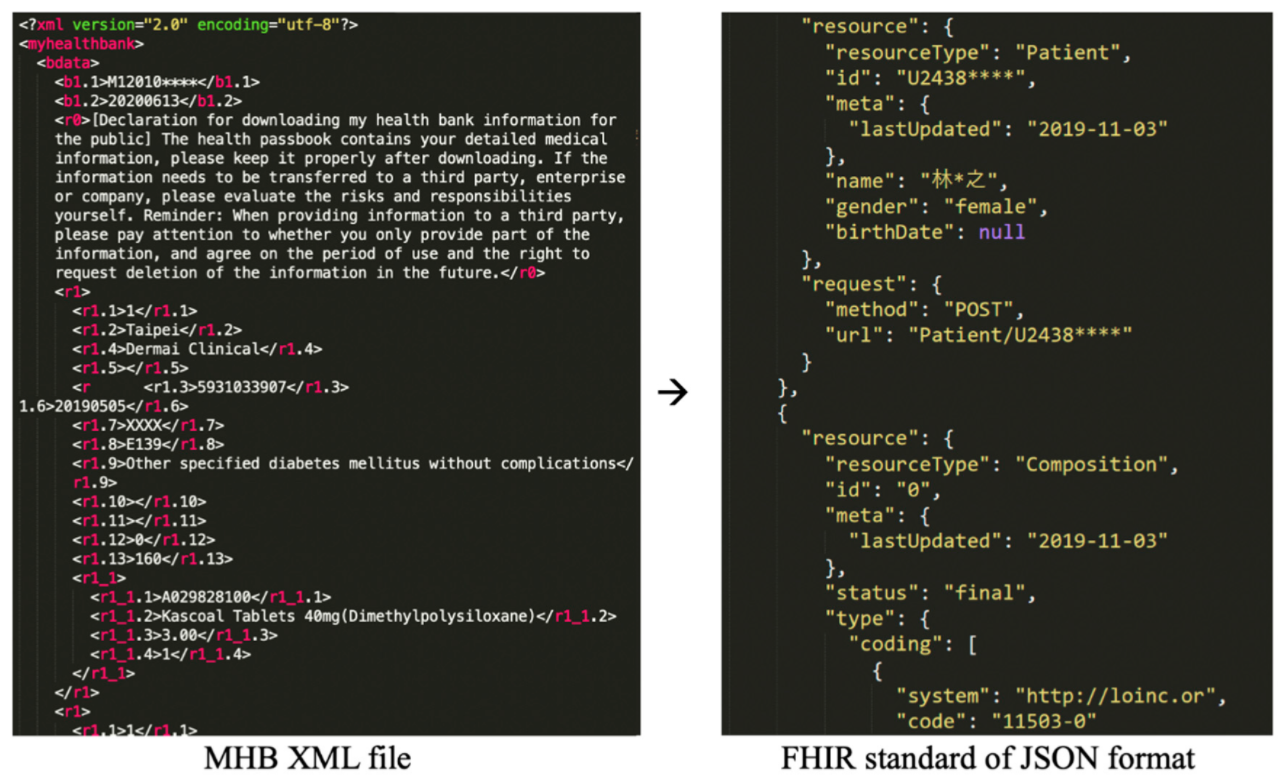
Each MHB has a total of three years of health insurance payment information. The information is presented as a single payment item by the unit. Figure 2 provides an example of a patient visit to a doctor on October 20, 2019 (20191020). Not that section b1.1 is personal national ID, b1.2 is the date of MHB create, r1.1 is the number of record, r1.2 is the clinic location, r1.3 is the ID of clinic, r1.4 is the name of clinic, r1.8 is the International Classification of Disease (ICD) code of diagnosis, r1.9 is the Chinese name of diagnosis, r1.12 is the payment of national health insurance, r1.13 is the co-payment of patient, and r1_1 is the medical and medication order of this diagnosis. This represents a slice of information for a single patient’s medical treatment. In the MHB, the medical information for each medical visit for three years is distinguished and presented in different sections.
|
FHIR resource correspondence
The format of MHB is different to the structure that decomposes FHIR into separate resources. MHB does not correlate the contents of the data for each single visit. For example, when a patient goes to see a doctor for a fever, the clinical information (medical institution details, medical date, disease diagnosis, personal payment amount, health insurance payment points, and prescription details) will be stored in the same section. However, the information between the same section is not connected. The next time the patient goes to see the doctor, a new section will be created. During FHIR-format data storage, each piece of data needs to be concatenated and referenced to the other pieces of data. In the future, data search and management efficiency can greatly improve.
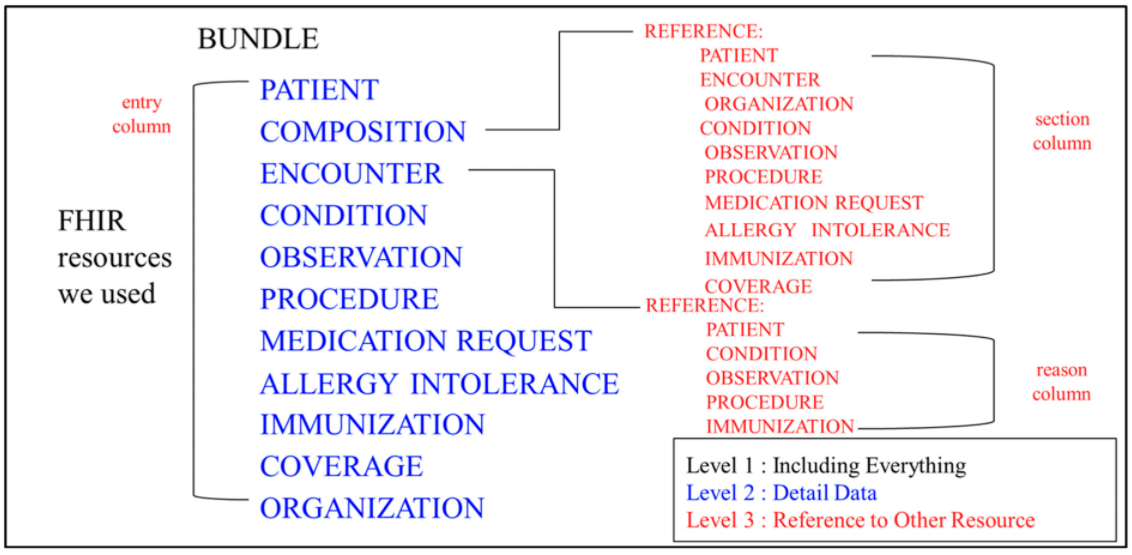
This study provided FHIR-based personal health records and designed a FHIR-based personal health management platform. FHIR “Bundle” is used to combine whole data into one document. FHIR Bundle is a resource that gathers a collection of different resources into a single document. We used it to bundle resources together as a single health record.
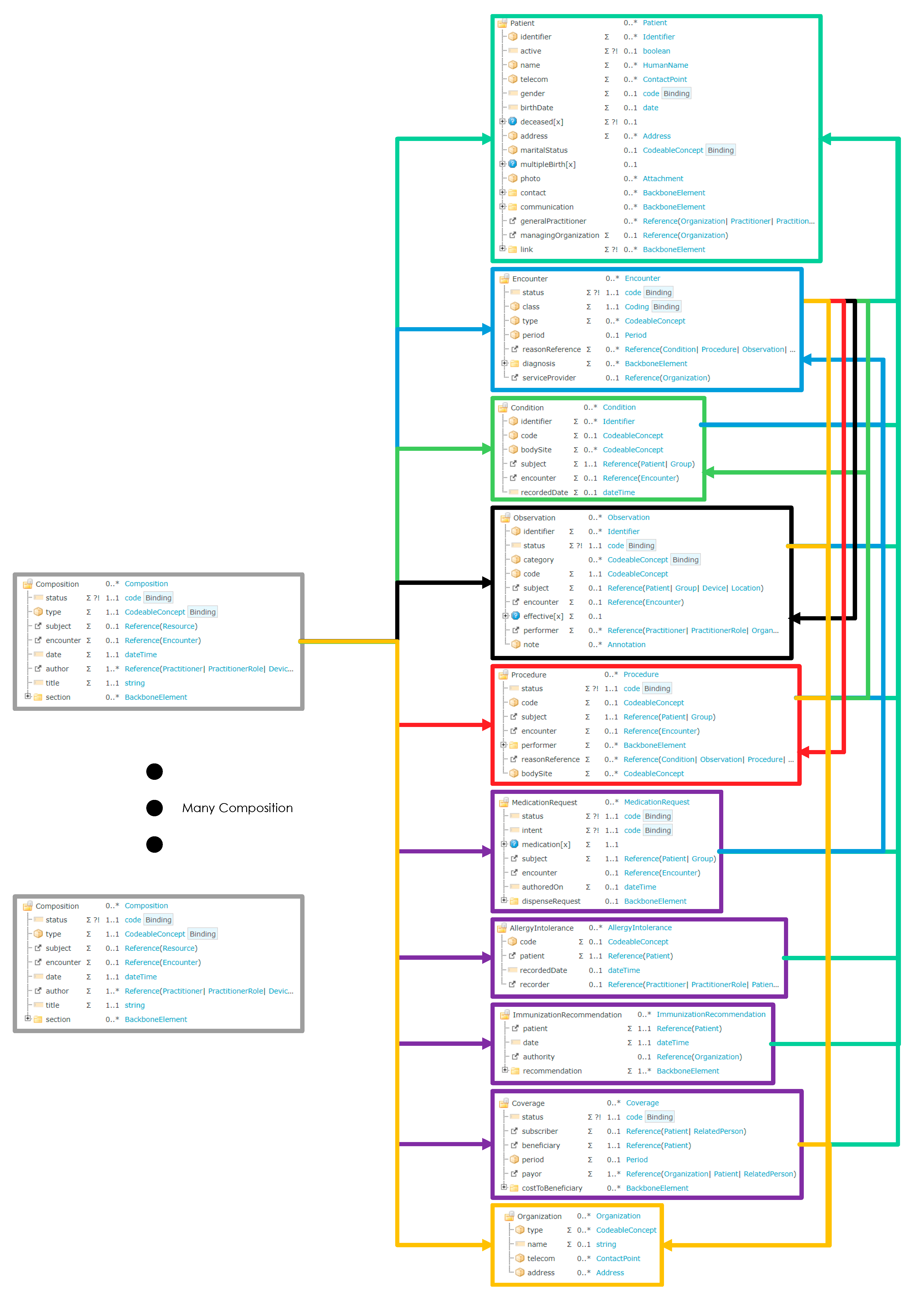
The structure of the conversion of the health passbook into the FHIR format in this study is shown in Figure 3. The FHIR structure uses a three-tier design for format conversion. The first layer (black) uses the Bundle resource to integrate all the information of the MHB. The second layer (blue) uses a total of 11 different resources to store the detailed information of the MHB according to the information contained in the health passbook. The third layer (red) is the index between each data. In FHIR, the data will be scattered everywhere and then linked to each other by index to ensure that the data is complete and easy to retrieve.
|
A composition resource is a set of healthcare-related information that can connect all single pieces of information for one medical service and has clinical attestation.
In this study, composition resources were used to connect records with different pieces of data. The composition resources included patient information (reference to patient resources), medical institution details (reference to organization resources), medical service information (reference to encounter resources), disease diagnoses (reference to condition resources), personal payment amounts (reference to coverage resources), health insurance payment points (reference to coverage resources), treatment details (reference to procedure resources), prescription details (reference to medication request resources), and testing reports (reference to observation resources).
The FHIR Encounter resource was used to record the interaction between patient and healthcare provider. The data include healthcare services records and the medical service place.
The Encounter resource was used to record the information of each medical service, including clinical diagnoses, observations, medical procedures, and immunizations (reference to different resources). Due to the different structures of MHB and the FHIR format, it cannot connect the medication information to the Encounter resource directly. In our design, the Encounter resource was connected to the Composition resource for connecting all information.
The PHR from a different country should be converted to the same standard for cross-country interoperability PHR implementation. FHIR Release #4 (version 4.0.1) was implemented in this study.
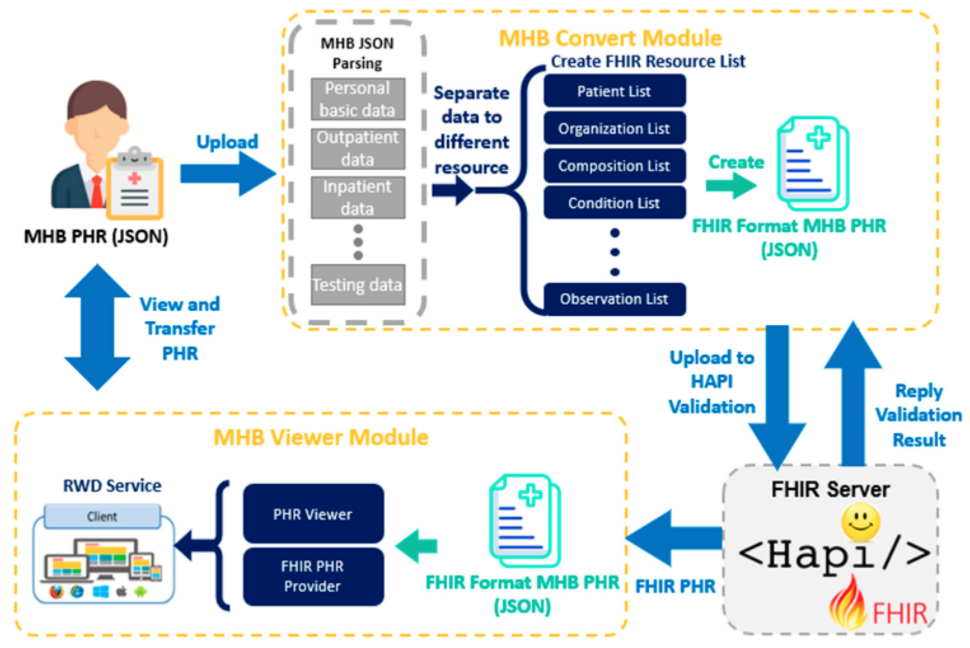
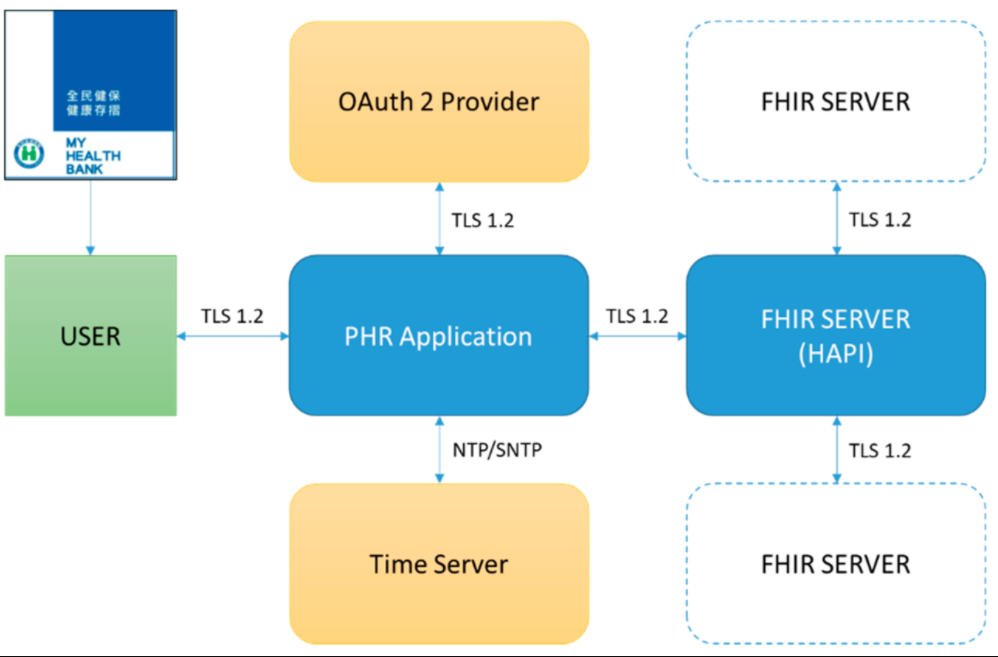
Personal health record management platform design
A platform was developed to view and transform PHRs. The platform contained two main modules. The architecture of the platform and module is shown in Figure 4. The MHB conversion module was used to convert the MHB data downloaded from the NHIA to the FHIR format. The index in the MHB was parsed and mapped to a separate FHIR resource. After data processing, an FHIR-format PHR could be created through this module. An HL7 application programming interface (HAPI) FHIR server was used as a health data server in our platform. HAPI FHIR is an open-source code that can fully implement the FHIR standard for interoperability in healthcare. It can store health data that comply with the FHIR format. Health data can be managed and transmitted based on a HAPI server, and HAPI can be used to verify the correctness of the FHIR format. If the format is not FHIR-compliant, the upload will be rejected.
|
The PHR viewer module could be used to view and manage personal health records, and PHR JSON files based on the FHIR format could be transferred by the viewer module.
For the design of data interoperability, the files after FHIR format conversion through the platform can be downloaded from the platform. The development of this research platform uses Windows 10 as the basic environment, and uses ASP.NET to set up a front visualization display platform and a back-end database data transmission and acceptance platform. The database uses a HAPI Server.
Authentication and security
The architecture of authentication and security mechanism in this platform is shown in Figure 5. Network Time Protocol (NTP)/Simple Network Time Protocol (SNTP) was used in the security and user authentication mechanism when processing and applying personal health information. The correct time was sourced from the National Time and Frequency Standard Laboratory. Transport Layer Security (TLS) 1.2 (such as HTTP Secure (HTTPS)) was used for protection in the data communication part. TLS 1.2 was released in 2008 and can operate on HTTP/2. Currently, mainstream browsers only implement encrypted HTTP/2, which makes HTTP/2 + TLS 1.2 or later a mandatory standard.
|
User authentication is a critical part in this platform. Confirmation of legitimate user access can ensure data security. Referring to HL7 official recommendations, we used OAuth (OAuth 2.0) in the user authentication mechanism. OAuth2 is an authorization framework that allows users access to the user’s private resources (such as photos, videos, and contact lists) stored on a certain website without a username and password through a third-party application. Third-party applications can obtain limited access to user accounts on OAuth2 providers (such as Microsoft, Google, Facebook, or Twitter) through HTTP/HTTPS services.
This system does not verify the user itself (such as account/password), but uses it in the OAuth2 environment where the OAuth2 provider is responsible for user authentication. Usually, when a user wants to log into the system, it will interactively redirect the user to the OAuth2 provider for authentication and obtain an OAuth2 token. Then, it sends back the HTTP request and provides the OAuth2 token in the HTTP Authentication header to represent the user. The system obtains the OAuth2 token and uses the OAuth2 authorization server to verify it and complete the login. In this way, system users can use accounts from Microsoft, Google, Facebook, or Twitter to log in with existing verification procedures, and only after logging into the system can they be associated with user data in the system.
Results
Interoperability PHR: Profile of MHB PHR based on FHIR format
The MHB PHRs based on FHIR format were implemented in this study. A total of 11 resources were included in our PHRs, including patients, composition, encounters, conditions, observations, procedures, medication requests, allergy intolerances, immunization recommendations, coverage, and organizations. The MHB data were converted to the FHIR format and stored in the personal health management platform.
The Bundle resource was used to connect the whole records. Different resources could be referenced through the subject element, which integrated the entire medical record of each medical service under the Composition resource. The Patient resource included personal information such as name, telephone number, gender, birthday, and address.
Encounter resource data referred to medical service information, including diagnoses and service providers, and could be referenced to Condition, Procedure, Observation, Condition, Patient, and Organization. Condition resource data referred to diagnoses and could be referenced to Encounter and Patient. Observation data referred to testing reports, including type of testing and value, and could be referenced to Organization, Patient, and Encounter. Procedure referred to treatment details and could be referenced to Patient, Encounter, and Condition. Medication request data referred to prescription details, including the drug, dosage, and code, and could be referenced to Patient and Encounter. Allergy intolerance data referred to allergy information and could be referenced to Patient. Coverage data referred to payment information, including personal payment amounts and health insurance payment points, and could be referenced to Patient and Encounter. Organization data referred to organization information, including name, telephone number, and address. The structure of different resource connections is shown in Figure 6.
|
In Figure 6, each box represents a different resource. We converted the MHB single medical service record into a data format that conforms to the FHIR framework to meet international standards and subsequent data management applications.
The box representing each resource describes the relevant data that can be stored and the amount of data that can be stored. Take the composition resource on the left in Figure 5 as an example: it can contain different items of status, type, subject, encounter, date, author, title, and section. The field “0..*” means the amount of different data that can be stored. Take status as an example: the content of the field “0..*” is “1..1”, which means the status must have a data point and only can have one data point. Take section as another example: the content of the field “0..*” is “0..*”, which means that there can be no section data, or an unlimited number of sections (* means unlimited number).
Data conversion of international format
The conversion result of the MHB XML file into the FHIR standard of JSON format is shown in Figure 7. The different types of forms in the MHB were disassembled into different types of FHIR. According to the data format of each medical visit record in the MHB, the relevant data are referenced to the Composition resource. Each resource is also referenced to others.
|
For example, the Encounter resource references all information about patient medical records, including resources such as Patient, Condition, Observation, Procedure, and Organization. Therefore, the information of each record can be retrieved from the Encounter resource. However, according to the FHIR standard, Encounter cannot reference medication and medical orders, so the Composition resource is used to concatenate the medication and treatment orders of each record to achieve the correlation between the data.
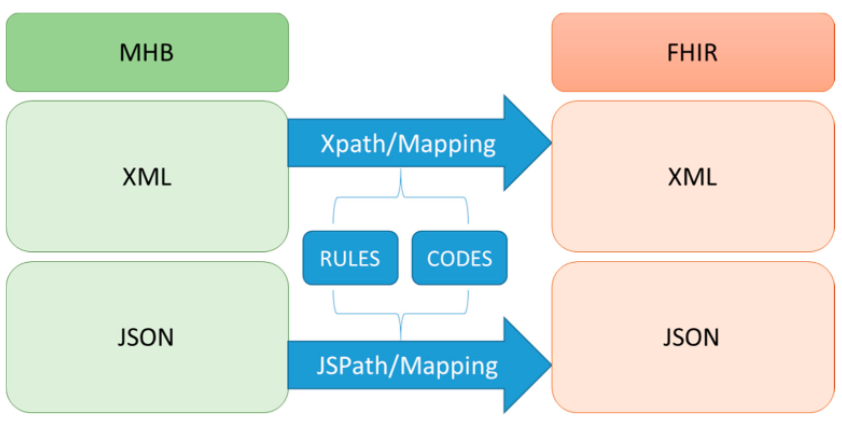
The main core of the data conversion module is the use of custom filters and conversion template technology. The data conversion module architecture is shown in Figure 8. Since the source data format of MHB can be XML or JSON, XPath and JSPath technologies are applied to filter out specific information modules. Then, we combined the corresponding defined MHB and FHIR format mapping logic template for conversion. In the template, items/attributes, coding, and even logic rules are described for the information modules of the source and target. Through this model, whether it is a new version or a new item of MHB or a new version of FHIR in the future, resources can be easily mapped, and FHIR data (XML/JSON) conforming to the latest specifications can be successfully produced.
|
Personal health management platform
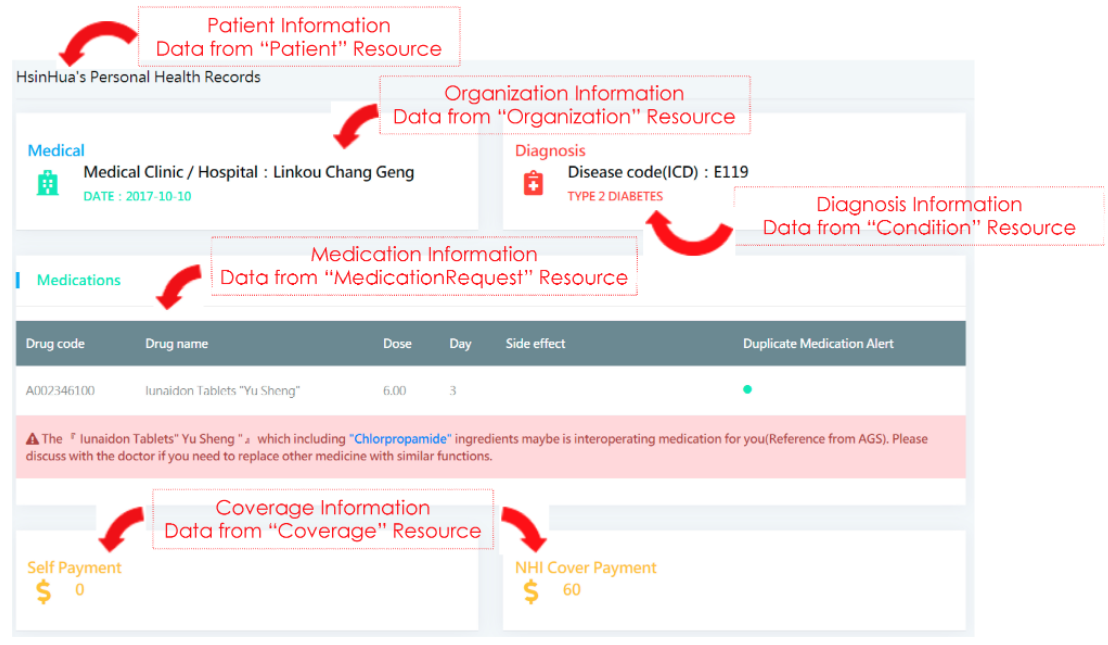
After the user uploads the MHB data to the platform, the PHRs will be automatically converted to the FHIR format. PHR data can be displayed in a platform for personal health management. An example of a personal health record and user interface is shown in Figure 9. Record examples include patient information, diagnoses, service provider organization information, medication information, and coverage. Health records in the FHIR format can be displayed and stored on the platform, and users can download PHRs in FHIR format for record management or data exchange. The platform has achieved international interoperability goals, and data exchange efficiency and high quality can be improved through the platform.
|
Data verification mechanism
After the data are converted, the correctness of the data format needs to be verified. A HAPI server is used in the data verification mechanism.
HAPI is open-source software designed by a group of experts in the medical information field. Its architecture complies with FHIR standards and procedures. It has end-to-end code hygiene, secure defaults, regular updates, advanced features, reliability, predictable ownership, and in-house security features of expertise. After the HAPI server is established, data can be uploaded in an FHIR-compliant form.
In the data conversion process of this research, the converted FHIR JSON file was sent to the HAPI server to confirm that it is correct before the entire file was saved and output.
Discussion
The interoperability of the PHR format and international data exchange are essential in any kind of medical service. The interoperability of standards-based communication of system issue was previously analyzed by Urbauer et al.[12] They discussed the gaps in system interoperability communication and suggested possible solutions. Alyami et al.[9] and Roehrs et al.[13] proposed the key point of interoperability of personal health records. A service-oriented architecture for developing an interoperable integrated PHR system was presented by Li.[11] And Roehrs et al.[27] proposed an application model for integrating different standards in PHRs to solve the interoperability problem.
Although many studies have discussed interoperability, it is inefficient to design a unique system for each different topic and goal. The HL7 FHIR achieved interoperability and system development efficiency by taking a different approach. Instead of using traditional data storage methods, HL7 FHIR uses a modular approach separating healthcare and medical service data (such as patient information, diagnoses, treatments, medications, and service records, etc.) into independent modules, which are called resources. The FHIR record control architecture is based on APIs and RESTful web services (the backbone of modern web applications) to achieve efficient and interoperable PHR control by utilizing modern web and mobile technology designs (such as HTTP-based lightweight REST protocol, JSON, or RDF, etc.).
According to the research of Saripalle et al.[37], FHIR can be used as the basic structure of PHR and has the ability to customize the PHR. At present, Taiwan does not have any data that meet international standards and regulations, which leads to a gap in international medical treatment. In the era of globalization, data should be integrated and applied as soon as possible to improve the convenience of data exchange, access, and use.
On the other hand, under the application of data analysis and big-data-related artificial intelligence (AI), more and more attention is paid to data conforming to international standards, and only data conforming to standards can be quickly integrated and applied. Real-world evidence (RWE) research, for example, needs to ensure that key results of effectiveness can be observed and established in real-world data (RWD) sources, and a clinical RWD database can provide correct data to affect the overall research design and its clinical and cost burden. It may be necessary for a data repository to incorporate new data with the FHIR international format into the PHR or to collect and store biomarkers for subsequent analysis. In clinical research, studies such as the Salford Lung Study[38] have proven that the use of RWD data can make potential progress in generating RWE, but it has also found many challenges related to infrastructure and research funding resources.
Conclusion
Although many studies have made clinical data management systems that meet international standards, most of them are based on patients with specific diseases, and data interoperability is still inflexible. The innovation of this research is to take personal health records as the main body of the contents and apply international standards to establish a demonstration platform. Through the integration of different technologies—such as Xpath and JSPath for data conversion, HAPI server for data verification, and OAuth for authentication—an interoperable platform with personal health records as the main body has been constructed.
This study leveraged HL7 FHIR to achieve interoperability as well as capture and share data using FHIR resources and formats. Taiwan’s My Health Bank personal health records, launched by the NHI, was used as an international prototype. Our platform can perform personal health control and data management and provide PHRs based on FHIR. Users can exchange PHRs easily and efficiency. Based on the FHIR format, the platform can not only provide PHRs in the FHIR format but also capture any healthcare data based on FHIR. The main purposes of the platform were to demonstrate the content of HL7 FHIR resources and personal health information (profiles, health records, and functional standards) and to design and implement interoperable PHRs that are compatible with HL7 PHRs. The HL7 FHIR was a specification and standard, and the HAPI FHIR, which is a Java implementation of HL7 FHIR, was used as the database. The data captured in the PHR were structured as an FHIR resource and shared with the EHR in the JSON format using web services. The conversion of data was verified by HAPI in the correct format, and it was provided for users to download and view on website services. In general, this study allowed PHRs to be interoperable and easily exchanged and an architecture for international data exchange to be proposed.
Comparing our study to other studies, the degree of interoperability is higher and the applicable population is larger (not confined by specific health problems). There are very few restrictions to adopting our platform since we use HL7 FHIR and all other open-source resources, and the personal health management can be implemented since the MHB provides most of the information we need to do health management. Our platform provides a user-friendly authentication process based on the OAuth mechanism. Therefore, in this study, we have completed an innovative application framework in Taiwan. The application we developed will be very useful for a single person to use or for other system developers to implement their own standard PHR software.
Acknowledgements
Author contributions
Conceptualization, Y.-L.L., H.-A.L., and C.-Y.H.; methodology, Y.-L.L. and H.-A.L.; software, H.-H.K.; validation, H.-A.L.; system structure design, Y.-L.L. and H.-A.L.; writing—original draft preparation, Y.-L.L. and H.-A.L.; writing—review and editing, C.-Y.H. and H.-W.C.; supervision, H.-W.C. All authors have read and agreed to the published version of the manuscript.
Funding
This research was funded by Ministry of Science and Technology, Taiwan grant number 109-2221-E-227 -003 -MY2.
Conflicts of interest
The authors declare no conflict of interest.
References
- ↑ Tang, P.C.; Ash, J.S.; Bates, D.W. et al. (2006). "Personal health records: definitions, benefits, and strategies for overcoming barriers to adoption". JAMIA 13 (2): 121–6. doi:10.1197/jamia.M2025. PMC PMC1447551. PMID 16357345. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1447551.
- ↑ Markle Foundation (1 July 2003). "Connecting for Health: A Public-Private Collaborative" (PDF). Markle Foundation. https://www.markle.org/sites/default/files/final_phwg_report1.pdf. Retrieved 10 March 2021.
- ↑ Bower, J.K.; Bollinger, C.E.; Foraker, R.E. et al. (2017). "Active Use of Electronic Health Records (EHRs) and Personal Health Records (PHRs) for Epidemiologic Research: Sample Representativeness and Nonresponse Bias in a Study of Women During Pregnancy". EGEMS 5 (1): 1263. doi:10.13063/2327-9214.1263. PMC PMC5340503. PMID 28303255. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5340503.
- ↑ Bonanader, J.; Gates, S. (2010). "Public health in an era of personal health records: Opportunities for innovation and new partnerships". Journal of Medical Internet Research 12 (3): e33. doi:10.2196/jmir.1346. PMC PMC2956336. PMID 20699216. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2956336.
- ↑ Timmerman, L. (4 February 2013). "What’s in a Name? A Lot, When It Comes to ‘Precision Medicine’". Xconomy. https://xconomy.com/national/2013/02/04/whats-in-a-name-a-lot-when-it-comes-to-precision-medicine/.
- ↑ Ireland, S. (5 August 2019). "Revealed: Countries With The Best Health Care Systems, 2019". CEOWORLD magazine. https://ceoworld.biz/2019/08/05/revealed-countries-with-the-best-health-care-systems-2019/.
- ↑ Iqbal, U.; Nguyen, P.-A.; Syed-Abdul, S. et al.. Is long-term use of benzodiazepine a risk for cancer?. 94. e483. doi:10.1097/MD.0000000000000483. PMC PMC4602739. PMID 25674736. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4602739.
- ↑ Jung, S.Y.; Lee, K.; Hwang, H. et al. (2017). "Support for Sustainable Use of Personal Health Records: Understanding the Needs of Users as a First Step Towards Patient-Driven Mobile Health". JMIR mHealth and uHealth 5 (2): e19. doi:10.2196/mhealth.6021. PMC PMC5344982. PMID 28232300. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5344982.
- ↑ 9.0 9.1 Alyami, M.A.; Song, Y.-T. (2016). "Removing barriers in using personal health record systems". Proceedings of the 2016 IEEE/ACIS 15th International Conference on Computer and Information Science: 1–8. doi:10.1109/ICIS.2016.7550810.
- ↑ Plastiras, P.; O'Sullivan, D.M. (2017). "Combining Ontologies and Open Standards to Derive a Middle Layer Information Model for Interoperability of Personal and Electronic Health Records". Journal of Medical Systems 41 (12): 195. doi:10.1007/s10916-017-0838-9. PMID 29081012.
- ↑ 11.0 11.1 Li, J. (2017). "A Service-Oriented Approach to Interoperable and Secure Personal Health Record Systems". Proceedings of the 2017 IEEE Symposium on Service-Oriented System Engineering. doi:10.1109/SOSE.2017.20.
- ↑ 12.0 12.1 Urbauer, P.; Sauermann, S.; Frohner, M. et al. (2015). "Applicability of IHE/Continua components for PHR systems: Learning from experiences". Computers in Biology and Medicine 59: 186–93. doi:10.1016/j.compbiomed.2013.12.003. PMID 24374230.
- ↑ 13.0 13.1 Roehrs, A.; da Costa, C.A.; da Rosa Righi, R. et al. (2017). "Personal Health Records: A Systematic Literature Review". Journal of Medical Internet Research 19 (1): e13. doi:10.2196/jmir.5876. PMC PMC5251169. PMID 28062391. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5251169.
- ↑ "Welcome to FHIR". Health Level 7. 1 November 2019. https://hl7.org/FHIR/. Retrieved 26 April 2020.
- ↑ Schleyer, T.K.L.; Rahurkar, S.; Baublet, A.M. et al. (2019). "Preliminary evaluation of the Chest Pain Dashboard, a FHIR-based approach for integrating health information exchange information directly into the clinical workflow". AMIA Joint Summits on Translational Science 2019: 656-664. PMC PMC6568135. PMID 31259021. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6568135.
- ↑ Goodman, A.B.; Braun, P.; Braunstein, M. (2018). "Healthy Weight on FHIR - Innovative Technology to Support High Quality Clinical Care & Clinical to Community Linkages for Child Obesity". PEdiatrics 141 (1 MeetingAbstract): 12. doi:10.1542/peds.141.1_MeetingAbstract.12.
- ↑ Baihan, M.S.; Sánchez, Y.K.R.; Shao, X. et al. (2018). "Chapter 6: A Blueprint for Designing and Developing M-Health Applications for Diverse Stakeholders Utilizing FHIR". In Rajkumar, R.. Contemporary Applications of Mobile Computing in Healthcare Settings. IGI Global. pp. 85–124. doi:10.4018/978-1-5225-5036-5.ch006. ISBN 9781522550365.
- ↑ Daumke, P.; Heitmann, K.U.; Heckmann, S. et al. (2019). "Clinical Text Mining on FHIR". Studies in Health Technology and Informatics 264: 83–7. doi:10.3233/SHTI190188. PMID 31437890.
- ↑ Storck, M.; Hollenberg, L.; Dugas, M. et al. (2019). "Interoperability Improvement of Mobile Patient Survey (MoPat) Implementing Fast Health Interoperability Resources (FHIR)". Studies in Health Technology and Informatics 258: 141–45. PMID 30942732.
- ↑ Giordanengo, A.; Bradway, M.; Grøttland, A. et al. (29 August 2017). "A FHIR-based Data Flow Enabling Patients with Diabetes to Share Self-collected Data with the Norwegian National Healthcare Systems and Electronic Health Records Systems" (PDF). 2017 Scandinavian Conference on Health Informatics. Norwegian Centre for E-health Research. https://ehealthresearch.no/files/documents/Postere/Poster_2018-02_16-9-ATTD-FHIR-based-Data-Flow.pdf.
- ↑ Kiourtis, A.; Mavrogiorgou, A.; Menychtas, A. et al. (2019). "Structurally Mapping Healthcare Data to HL7 FHIR through Ontology Alignment". Journal of Medical Systems 43 (3): 62. doi:10.1007/s10916-019-1183-y. PMID 30721349.
- ↑ Gøeg, K.R.; Rasmussen, R.K.; Jensen, L. et al. (2018). "A future-proof architecture for telemedicine using loose-coupled modules and HL7 FHIR". Computer Methods and Programs in Biomedicine 160: 95–101. doi:10.1016/j.cmpb.2018.03.010. PMID 29728251.
- ↑ Alper, B.; Mayer, M.; Shahin, K. et al. (2019). "Achieving evidence interoperability in the computer age: Setting evidence on FHIR". BMJ Evidence-Based Medicine 24 (Suppl. 1): A15. https://ebm.bmj.com/content/24/Suppl_1/A15.1.
- ↑ Lackerbauer, A.M.; Lin, A.C.; Krauss, O. et al. (2018). "A Model for Implementing an Interoperable Electronic Consent Form for Medical Treatment Using HL7 FHIR". European Journal for Biomedical Informatics 14 (3): 37–47. doi:10.24105/ejbi.2018.14.3.6.
- ↑ Dixon, B.E.; Taylor, D.E.; Choi, M. et al. (2019). "Integration of FHIR to Facilitate Electronic Case Reporting: Results from a Pilot Study". Studies in Health Technology and Informatics 264: 940–44. doi:10.3233/SHTI190362. PMID 31438062.
- ↑ Hussain, M.A.; Langer, S.G.; Kohli, M. et al. (2018). "Learning HL7 FHIR Using the HAPI FHIR Server and Its Use in Medical Imaging with the SIIM Dataset". Journal of Digital Imaging 31 (3): 334–40. doi:10.1007/s10278-018-0090-y. PMC PMC5959839. PMID 29725959. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5959839.
- ↑ 27.0 27.1 Roehrs, A.; da Costa, C.A.; da Rosa Righi, R. et al. (2019). "Toward a Model for Personal Health Record Interoperability". IEEE Journal of Biomedical and Health Informatics 23 (2): 867–73. doi:10.1109/JBHI.2018.2836138. PMID 29993759.
- ↑ Martínez-García, A.; García-García, J.A.; Escalona, M.J. et al. (2015). "Working with the HL7 metamodel in a Model Driven Engineering context". Journal of Biomedical Informatics 57: 415–24. doi:10.1016/j.jbi.2015.09.001. PMID 26348545.
- ↑ Walderhaug, S.; Stav, E.; Mikalsen, M. (2008). "Experiences from Model-Driven Development of Homecare Services: UML Profiles and Domain Models". Proceedings of MODELS 2008: International Conference on Model Driven Engineering Languages and Systems: 199–212. doi:10.1007/978-3-642-01648-6_22.
- ↑ González-Ferrer, A.; Peleg, M.; Verhees, B. et al. (2012). "Data integration for clinical decision support based on open EHR archetypes and HL7 virtual medical record". In Lenz, R.; Miksch, S.; Peleg, M. et al.. Process Support and Knowledge Representation in Health Care. Springer. pp. 71–84. doi:10.1007/978-3-642-36438-9. ISBN 9783642364389.
- ↑ Simon, S.K.; Anbananthen, K.S.M.; Lee, S. (2013). "A Ubiquitous Personal Health Record (uPHR) Framework". Proceedings of the 2013 International Conference on Advanced Computer Science and Electronics Information: 423–27. doi:10.2991/icacsei.2013.105.
- ↑ Marceglia, S.; Fontelo, P.; Rossi, E. et al. (2015). "A Standards-Based Architecture Proposal for Integrating Patient mHealth Apps to Electronic Health Record Systems". Applied Clinical Informatics 6 (3): 488-505. doi:10.4338/ACI-2014-12-RA-0115. PMC PMC4586338. PMID 26448794. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4586338.
- ↑ Fonda, S.J.; Kedziora, R.J.; Vigersky, R.A. et al. (2010). "Evolution of a web-based, prototype Personal Health Application for diabetes self-management". Journal of Biomedical Informatics 43 (5 Suppl.): S17–21. doi:10.1016/j.jbi.2010.05.006. PMID 20937479.
- ↑ Backonja, U.; Kim, K.; Casper, G.R. et al. (2012). "Observations of daily living: putting the "personal" in personal health records". Proceedings of the 11th International Congress on Nursing Informatics 2012: 6. PMC PMC3799183. PMID 24199037. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3799183.
- ↑ Ferguson, G.; Quinn, J.; Horwitz, C. et al. (2010). "Towards a Personal Health Management Assistant". Journal of Biomedical Informatics 43 (5 Suppl.): S13–16. doi:10.1016/j.jbi.2010.05.007. PMID 20937478.
- ↑ Siek, K.A.; Ross, S.E.; Khan, D.U. et al. (2010). "Colorado Care Tablet: The design of an interoperable Personal Health Application to help older adults with multimorbidity manage their medications". Journal of Biomedical Informatics 43 (5 Suppl.): S22–6. doi:10.1016/j.jbi.2010.05.014. PMID 20937480.
- ↑ Saripalle, R.; Runyan, C.; Russell, M. (2019). "Using HL7 FHIR to achieve interoperability in patient health record". Journal of Biomedical Informatics 94: 103188. doi:10.1016/j.jbi.2019.103188. PMID 31063828.
- ↑ Bakerly, N.D.; Woodcock, A.; New, J.P. et al. (2015). "The Salford Lung Study protocol: A pragmatic, randomised phase III real-world effectiveness trial in chronic obstructive pulmonary disease". Respiratory Research 16 (1): 101. doi:10.1186/s12931-015-0267-6. PMC PMC4558879. PMID 26337978. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4558879.
Notes
This presentation is faithful to the original, with only a few minor changes to presentation. In some cases important information was missing from the references, and that information was added. The original reference 12 (Crabtree et al.) seems to have no bearing on the text and appears to have been accidentally included; it was omitted for this version. The same conclusion was reached about the original reference 38, which has also been omitted.