Difference between revisions of "LII:The Comprehensive Guide to Physician Office Laboratory Setup and Operation/The clinical environment"
| Line 107: | Line 107: | ||
The above diagram shows the typical workflow for POL data management. While managing this workflow is important, the data associated with it go beyond ordinary practice function; these data can be used to assist with tracking population health for the patients or be combined with financial data such as billing or spending on supplies. | The above diagram shows the typical workflow for POL data management. While managing this workflow is important, the data associated with it go beyond ordinary practice function; these data can be used to assist with tracking population health for the patients or be combined with financial data such as billing or spending on supplies. | ||
Other data streams may be generated outside this typical workflow as well. Meaningful Use Stage 3 will eventually require EHRs to accept patient-generated data. | Other data streams may be generated outside this typical workflow as well. Meaningful Use Stage 3 will eventually require EHRs to accept patient-generated data. These data can come from tracking tools like Fitbits or from glucometers used by the patient.<ref name="Fitbit">{{cite web |url=http://www.darkdaily.com/physicians-use-fitness-trackers-to-monitor-patients-in-real-time-even-as-developers-work-to-incorporate-medical-laboratory-tests-into-the-devices-528 |title=Physicians Use Fitness Trackers to Monitor Patients in Real-time, Even as Developers Work to Incorporate Medical Laboratory Tests into the Devices |author=McLeod, Pamela Scherer |work=Dark Daily |publisher=Dark Intelligence Group, Inc |date=19 March 2015 |accessdate=14 April 2015}}</ref> Such data can aid the physician with diagnosis by giving them more data points to examine, but this may also impact the data management methods of the practice. | ||
This area is a future frontier in the quest to use technology as a means of improving outcomes while driving costs down. The popularity of these patient devices and the trend towards using technology for healthcare purposes is drawing physician interest in using such devices for expanded monitoring of patients, with indicators supporting this trend on the development side.<ref name="Fitbit" /> The Scanadu Scanaflo, which "measures up to 12 reagents" as well as pH, represents another such device. Scanaflo is still in development, but it will work with a smartphone app and allow patients to monitor many areas of their health from home.<ref name="ScanTC" /> Results can be stored and interpreted via the app, and that data can eventually make its way into a physician's Stage 3-compliant EHR. (An interesting video about generating data at home with Scanadu devices can be [https://www.youtube.com/watch?v=gSxNjTXfgBo viewed here].) | This area is a future frontier in the quest to use technology as a means of improving outcomes while driving costs down. The popularity of these patient devices and the trend towards using technology for healthcare purposes is drawing physician interest in using such devices for expanded monitoring of patients, with indicators supporting this trend on the development side.<ref name="Fitbit" /> The Scanadu Scanaflo, which "measures up to 12 reagents" as well as pH, represents another such device. Scanaflo is still in development, but it will work with a smartphone app and allow patients to monitor many areas of their health from home.<ref name="ScanTC" /> Results can be stored and interpreted via the app, and that data can eventually make its way into a physician's Stage 3-compliant EHR. (An interesting video about generating data at home with Scanadu devices can be [https://www.youtube.com/watch?v=gSxNjTXfgBo viewed here].) | ||
Revision as of 15:42, 8 December 2015
The physician office laboratory (POL) is a clinical laboratory that is owned, operated, and managed by a physician office. Definitions, as noted in The Practical Guide to the U.S. Physician Office Laboratory, vary from state to state, but this is a solid enough definition. Nearly 49 percent of all clinical laboratories in the U.S. were POLs according to Centers for Medicare and Medicaid Services statistics in July 2015.[1]
This second chapter on the topic of the clinical working environment has 10 sections.
2. The Clinical Environment
The clinical laboratory and its equipment
The POL is a clinical laboratory located in an ambulatory or outpatient care setting, specifically in the physician office. The clinical laboratory is used to test specimens from human patients to assist with the diagnosis, treatment, or monitoring of a patient condition. Testing in the clinical lab generally depends on three common methodologies to meet those goals: comparing the current value of a tested substance to a reference value, examining a specimen with microscopy, and detecting the presence of infection-causing pathogens.[2]
These three methodologies depend on clinical expertise from staff. Managerial staff like laboratory directors and laboratory department supervisors, for example, are responsible for the planning, management, and administration of the lab's operations as well as applying and enforcing quality systems and regulatory requirements. The lab itself is staffed with pathologists, cytotechnologists, histotechnologists, and clinical laboratory assistants, performing and interpreting specimen tests using one or more techniques.[3] Those methodologies and tests also require a wide variety of instruments and equipment. A histotechnologist will require a microtome to prepare a specimen for an anatomical pathology examination, and blood chemistry analyses depend on sample tubes, centrifuges, and blood analyzers. More advanced clinical laboratories performing molecular diagnostics techniques will use specialty tools like fluorescence microscopes and spectrometers. And all that equipment must meet manufacturing, testing, and calibration standards to ensure the utmost accuracy of tests.[4]
However, the clinical environment of the POL is somewhat different than your average reference or diagnostic lab that receives, processes, and reports on specimens en masse. The POL is typically a smaller operation, performing simple laboratory testing that can produce useful diagnostic data cheaply and rapidly. Rather than performing advanced pathology procedures that require specific equipment and expertise, the POL typically focuses on blood chemistry, urinalysis, and other testing domains that don't require significant resources and provide rapid results. This can be seen in Centers for Medicare and Medicaid Services statistics reported in July 2015 that show more than 61 percent of POLs in the U.S. are certified to provide CLIA-waived tests[1], "simple tests with a low risk for an incorrect result."[5] These "simple tests" don't require advanced equipment and highly-trained physicians. Urinalysis reagent strips, influenza nasal swabs, and whole blood mononucleosis kits are all CLIA-waived testing devices that can be used by well-trained phlebotomists, nurses, or laboratory assistants.[6] Some POLs opt to provide more advanced testing services, however, with nearly 23 percent of all POLs holding provider performed microscopy (PPM) certificates to perform moderate-level CLIA testing.[1] This allows POLs to perform moderate complexity tests like urine sediment analysis and the determination of "the presence or absence of bacteria, fungi, parasites, or cellular elements" in a specimen.[7] However, the majority of POLs remain smaller and simpler than their diagnostic lab counterparts.
Good laboratory practices
As previously stated, the ultimate goal of the clinical laboratory — and by extension, the POL — is to test specimens from human patients to assist with the diagnosis, treatment, or monitoring of a patient condition. This, of course, requires accurate results to ensure the best result. In the 1970s the U.S. Food and Drug Administration noted non-clinical laboratories in many cases conceived experiments poorly, failed to inform laboratory personnel of protocol, and didn't regard strict laboratory procedure to be necessary. This brought about the Good Laboratory Practice regulations in November 1976.[8][9] Clinical laboratories were not left out of improvements, however. Though the Clinical Laboratories Improvement Act of 1967 brought about some reforms to laboratory practices[10], the act wasn't doing enough by the mid-1980s. The regulations were revised and put into effect on October 31, 1988 as the Clinical Laboratory Improvement Amendments of 1988.[11] Known as CLIA, the regulations have helped shape the policy and procedure of clinical laboratories of all types, including how training and experience is gauged and documented, reagents are prepared, and quality control is approached.
Today in the U.S., like any other clinical lab, physician office laboratories must follow good laboratory practices to ensure the best outcomes for its associated patients. These practices must be engaged in at every stage of the laboratory testing process. During the initial test ordering process, for example, lab personnel must review orders for accuracy and seek verification from the physician if there are any questions. Following order entry, staff should complete a requisition and explain all preparation procedures to the patient. When the patient arrives, staff should use appropriate procedures and containers to collect the specimen(s) from the patient. Processing of the specimen should include proper storage, preservation (if required), labeling, and transportation. The POL must run quality control tests prior to testing the patient sample to ensure instruments are properly calibrated and appropriate testing proficiency is met. After test completion, a laboratory report is printed and the physician notified. Patients should also be notified per the policy of the physician practice. Disposal of laboratory waste is also part of good laboratory practice, as is proper documentation in the patient record regarding testing and results.[2]
Laboratory safety
Like any other laboratory, safety in the clinical laboratory is of vital importance. Good safety practices ensure the sample being tested is not contaminated, and they also protect the person doing the testing from infection or other issues resulting from exposure.
Quality control guidelines and standards ensure procedures are followed and equipment is checked, lowering specimen contamination risk and improving the accuracy of test results. Laboratory safety guidelines assist professionals with managing risk from biohazards, chemical hazards, or physical hazards that may be present in the laboratory. The two U.S government agencies that primarily set safety guidelines are the Centers for Disease Control and Prevention (CDC) and the Occupational Safety and Health Administration (OSHA). CDC training involves learning about the chain of infection and standard precautions for infection control, while OSHA biohazard training involves the blood borne pathogen standard (BBPS) as well as the exposure control plans and guidelines that promote staff health and safety. OSHA also requires training to deal with chemical hazards in the laboratory.[12][2]
Laboratories of any size must also deal with physical hazards such as obstructions, electrical equipment, fires, floods, and earthquakes. Preparing for these possible hazards in some cases can be as simple as ensuring a box is not placed where someone walking could trip over it. OSHA has numerous guidelines related to the physical hazard training, including how to conduct a fire drill. Other beneficial preparatory activities include organizing and documenting clearly labeled chemical inventories, providing clear access to material safety data sheets (MSDS), enacting a hazard communication program, and providing training on OSHA adherence protocols.[12][2]
The POL is not exempt from these quality control and safety considerations simply because it's smaller and simpler, however. It may not have the chemical stocks and testing hazards of a large diagnostic lab, but specimens must still be kept uncontaminated and procedures for using even the simplest of CLIA-waived test devices must be followed. Biohazards are still generated and must be treated appropriately using work-practice controls, personal protective equipment, and engineering controls. And bleach (sodium hypochlorite), one of the most prevalent chemicals in labs[13], must still be handled properly to ensure human safety and equipment longevity.[12][2]
Regulatory compliance: HIPAA and PPACA
Clinical laboratories must comply with the Health Insurance Portability and Accountability Act of 1996 (HIPAA). Among HIPAAs many goals is the desire to improve privacy and security protections for an individual's personal and identifying health information. As such, laboratories are required to implement measures that prevent unauthorized disclosure of and access to a patient's protected health information (PHI) in the laboratory. In the original implementation of HIPAA, this meant that laboratory staff were discouraged from giving laboratory test results to a patient without physician permission.[2] However, in February 2014, the Department of Health and Human Services wanted to encourage patients to take a more proactive approach to their own health care by giving them a mechanism to learn more about their own health. The HHS put into place an amendment to CLIA that became effective in April 2014, allowing patients to request laboratory results directly from a laboratory. Under the change, laboratories (including POLs) are now required to give patients their laboratory results within 30 days of a written request by the patient or authorized agent. Other safeguards related to patient data and HIPAA are still applicable.[14] However, it's still not clear how this change impacts the POL, by definition located in the physician's office. As such, the physician's office-based procedures for acquiring PHI also likely apply to the in-office laboratory.
Another federal statute that impacts laboratory testing is the Patient Protection and Affordable Care Act (PPACA), signed in 2010 by President Barack Obama. This law cut fees paid for laboratory testing and established accountable care organizations (ACOs). Both the cuts to the Medicare Clinical Laboratory Fee Schedule and the creation of ACOs (which may decrease laboratory testing volume[15]) present additional challenges to the laboratory — especially in the physician office — as economic concerns may cause a laboratory to no longer have incentive to offer some forms of testing.
Regulatory compliance: CLIA
In 1988 the Clinical Laboratory Improvement Amendments (CLIA) were passed as an amendment to the original 1967 legislature.[11] CLIA attempts to ensure the accuracy, reliability, and timeliness of test results regardless of where the test was performed. As part of this process, seven different criteria are used to gauge and assign one of three complexity levels to laboratory devices, assays, and examinations: high, moderate, and waived.[5][16] Clinical laboratories handling specimens originating from the U.S. and its territories must apply for a CLIA certificate that is appropriate for the type of testing it performs.
The POL largely conducts CLIA-waived tests, with 61.3 percent of all POLs in the U.S. running on a CLIA certificate of waiver as of July 2015.[1] These tests are recognized as simple to perform with a low risk of erroneous results and include among others urinalysis for pregnancy and drugs of abuse, blood glucose and cholesterol tests, and fertility analysis. Despite the simplicity of a wiaved test, it "needs to be performed correctly, by trained personnel and in an environment where good laboratory practices are followed."[17] As such, the Centers for Medicare and Medicaid Services (CMS) provides additional enforcement of labs with CLIA certificates of waiver, conducting on-site visits to approximately two percent of such labs to verify quality testing, regulatory compliance, and test appropriateness.[18] In some cases a POL may also offer moderate-level provider performed microscopy (PPM) testing (22.7 percent of all POLs as of July 2015[1]), depending on the office specialty.[2] To perform this type of testing in addition to waived testing, a PPM certificate is also required.
Since most POL testing is waived, anyone can be the laboratory director at a POL; however, some states have different requirements, so it is important to check with your local regulatory body when hiring staff for the laboratory. POLs that also incorporate PPM testing have different requirements for directors, who "must meet specific education, training and experience under subpart M of the CLIA requirements."[19] More information can be found regarding the CLIA complexity levels and what is required under each on the FDA's website, the references in this section, and the CLIA waived test list.
Point-of-care testing
The College of American Pathologists (CAP) defines point-of-care testing (POCT) as "any type of laboratory testing that takes place at or near where the patient is located."[20] Historically this sort of testing was mundane due to the nature of the available methods; however, today these tests have advanced to include tests such as glucose testing. POCT can be a nice addition to the POL, as it can allow patients to monitor themselves between visits. Like waived CLIA tests, POCT can also be performed by laboratory personnel. Both personnel and patients (those who use testing devices at home) must be trained on how to use POCT devices in order to get the most accurate results.[21][22]
Some POCT devices are gradually allowing the patient to send data from their instruments directly to the physician office. However, this is not always a straightforward procedure. As the CAP notes in its point-of-view on POCT, "interoperability should be developed or expanded ... to provide better oversight and incorporation of results into the electronic medical record."[20] As Meaningful Use Stage 3 rules for electronic health records (EHRs) — which will require the acceptance of patient generated data — go into effect in 2016, questions still remain about how interoperable POCT devices and EHRs will actually be. (This will be discussed in more detail in the data management section below).
Provider-performed microscopy testing
CLIA has approved some tests for the provider performed microscopy (PPM) level, a subcategory of the moderate complexity level. These tests must be of moderate complexity and require a microscope as the primary analysis tool, and they must be performed by a qualified physician or nurse practitioner in a set period of time with limited handling of the specimen for the utmost accuracy.[23] Eligibility of PPM tests is determined by CMS, and include wet mounted tissue examinations, semen analysis, certain mucous and nasal smears, and certain urinalyses.[24] (For the full list, consult the CMS-updated PDF file.)
These individual tests are useful to many POLs, though they have their own procedures and require the ability to focus and maintain the microscope at optimal performance level. Part of doing so is learning the structures of the microscope and how to use it. Since these procedures are performed by physicians or mid-level practitioners, the provider should be well trained in how to do this. They should be able to identify the parts of the microscope and understand how the lenses work. Knowledge of proper slide preparation is also vital, as improperly prepared slides can ruin an otherwise correctly performed PPMT procedure. In addition to an appropriate microscope, PPMT procedures require several other items, including immersion oil, lens paper, and tissue (lint free, soft).[2] Finally, though PPMT isn't regulated, the provider and laboratory personnel should carefully document quality assurance procedures for PPMT at regular intervals.[23] As noted previously, POLs that incorporate PPM testing have different requirements for laboratory directors than CLIA-waived labs, requiring a higher level of documented training and competence.[19]
CLIA market and industry trends
Clinical laboratory testing trends
With over 13 billion laboratory tests performed in the United States every year, laboratory testing is the highest volume medical activity in the country. Laboratory testing influences approximately two-thirds of all medical decisions, and this testing often directs far more expensive care. As these trends continue, the laboratory will likely become a coordinator for the patient and care team. The laboratory will serve as a facilitator for the patient and clinicians alike to receive not only test results but also education about those results. The laboratory will also assist the clinical team with test utilization, reporting those results into the EHR as well as maintaining them.[25]
Laboratory testing is in an upward trend, as seen with the growth of point-of-care testing and the patient-centered medical home (PCMH). Given the popularity of consumer products that track healthcare data, this trend should continue for years to come. One example of this is VeinViewer, which assists the phlebotomist with the location of veins and eliminates the painful process of sticking a patient more than once in an attempt to draw blood.[26] Other technologies are driving trends in this area, including in the testing domain, where for example tech start-up Scanadu has been working on a device than can measure your vitals and a urinalysis strip than can be analyzed with a mobile app.[27]
POL testing trends
The third installment of research firm Kalorama Information's Physician Office Laboratory Markets reported the number of POLs performing CLIA-waived in vitro diagnostic (IVD) testing increased an average annual rate of 3.8 percent from 2005 to 2013, though "the number of POLs conducting moderate and high complexity testing under CLIA compliance or accreditation decreased by an annual average rate of 0.8 percent."[28] In mid- to late 2014, Kalorama estimated that POLs were conducting nine percent of all clinical IVD testing in the United States, also noting that "[n]ine out of the ten most-performed POL tests in the United States are CLIA-waived."[29]
As for what's being tested, the report noted that "[i]n the past five years, the most performed POL tests have changed little with the exception of some recently CLIA-waived infectious disease tests and vitamin D testing."[28] The study also found that many of the CLIA waivers granted in 2014 have been for tests in "highly competitive, established POL segments, such as drugs-of-abuse testing, routine clinical chemistries, urinalysis, hormone tests (including pregnancy), and dipstick urinalysis."[30] Many of those IVD tests were likely waived by regulation or cleared for home or over-the-counter use; however, a few of those tests had to go through a more rigorous process to become CLIA-waived.
Addition of the Dual 510(k) and CLIA Waiver by Application process
Originally an IVD test product not CLIA-waived by regulation or not cleared for home or over-the-counter use — even if it had clear advantages as a CLIA-waived product — would have to first be taken through the FDA 510(k) premarketing submission process which would then classify it as moderate or high complexity.[31] Then, if the product was viable as a moderate complexity device, the manufacturer would try to market and make money on their product and then go through the CLIA Waiver by Application process if they thought there were clear benefits and eligibility for CLIA-waived product status. This process would work for many manufacturers but frustrate a few (as of 2014, only 10 to 12 CLIA Waiver by Application requests were arriving to the FDA each year) who deemed their product non-viable to market unless it were CLIA-waived.[32]
Initially driven by the Medical Device User Fee Amendments of 2012 (MDUFA III) — an FDA attempt "to increase the efficiency of regulatory processes in order to reduce the time it takes to bring safe and effective medical devices to the U.S. market"[33] — the FDA sought to overhaul its Administrative Procedures for CLIA Categorization guidance documents, tracking mechanisms, and public CLIA database to improve the IVD and medical equipment regulation process. Among these changes, effective March 21, 2014, was the addition of the Dual 510(k) and CLIA Waiver by Application process, specifically for "that small subset of products that are not really viable if they are not waived."[32][34][35] The process is specific, requiring a pre-submission to receive FDA feedback first and be cleared for the Dual strategy. If approved, both the 510(k) and the CLIA Waiver by Application can be submitted at the same time.[32][31][36] On December 17, 2014, rapid diagnostic manufacturer Quidel Corporation announced its Sofia Strep A+ Fluorescent Immunoassay became the first product to be approved through the Dual program[37], opening a potential gateway for other rapid diagnostic companies to fast-track their product through FDA and CLIA waiver approval.
More sophisticated CLIA-waived tests appear
More sophisticated tests eligible for labs with a certificate of waiver are appearing as of late, further increasing same-day testing opportunities in POLs. The first ever waived rapid screening test for syphilis was approved in the United States in December 2014, allowing physicians to make a preliminary diagnosis in as soon as 12 minutes. The product came about with the recognition of a the increasing number of primary and secondary syphilis cases in the U.S., nearly 55,000 new cases a year.[38] HIV testing is another growing segment of POL activities. Nearly four percent of all approved CLIA-waived tests are HIV tests, and of labs that offer CLIA-waived testing in general, 36 percent of them include at least one CLIA-waived HIV test.[39] The demand for more accurate and timely test results has driven companies like Trinity Biotech to create more flexible options; in November 2014 the company announced its Uni-Gold Recombigen HIV test "for the detection of antibodies to HIV in human serum, plasma, venous, and finger stick whole blood" was approved for CLIA-waived status, making it at the time the only rapid HIV test to be approved for all sample types.[40]
Several POCT companies have stepped up their CLIA-waived efforts recently, including Alere, Inc. and Cepheid, Inc. In an April 2015 interview with GenomeWeb, Cepheid chairman and CEO John Bishop stated the company would be "adding a sales force specifically for the CLIA market in early May" with expectations that the "market is actually going to step up overall test volumes as you move more broadly-disseminated."[41] Alere has been doing the same, though both companies are arguably heading up the charge towards a new potential trend in the CLIA-waived testing market: molecular and nucleic acid-based testing.
"I think the molecular tests are going to grab market share very rapidly ... and that's going to get even more emphasized with all of the programs now on antibiotic stewardship and more diagnostically directed use of therapeutics."[41] - John Bishop, Cepheid, Inc. chairman and CEO
"[W]e look forward to kind of changing the concept in the marketplace, [and showing] that you can get a highly sensitive, molecular result in minutes."[42] - K.C. McGrath, Alere, Inc. respiratory product manager
"We expect many other simple and accurate tests using nucleic acid-based technology to be developed in the near future. Once cleared by FDA, such tests can allow health care professionals to receive test results more quickly to inform further diagnostic and treatment decisions."[43] - Alberto Gutierrez, FDA director of the Office of In Vitro Diagnostics and Radiological Health
"I think traditional [polymerase chain reaction] assays will get better, faster, their boxes will get smaller, and you'll start to see a lot more point-of-care approved tests."[44] - Christine Ginocchio, BioMérieux vice president of global microbiology affairs
Molecular diagnostic tests have long been the domain of the full-fledged laboratory, even as companies like Cepheid have made progress with sales of its molecular Flu Xpert test[41], rated by CLIA for moderate complexity labs.[45] With only roughly 30 percent of physicians offices running at moderate complexity[42], however, molecular testing has seemed largely out-of-reach for the POL. Yet in January 2015, Alere and the FDA announced that the i Influenza A & B test had become the first ever nucleic acid-based test to receive CLIA-waived status, meaning it could be offered in POLs with a certificate of waiver.[45][43] While it's not clear if molecular point-of-care and and POL-friendly tests will become more prevalent in the coming years, their benefit to the POL are becoming clearer. In the case of the i Influenza A & B test, diagnosing a patient with influenza on a same-day physician visit with easy-to-use molecular tech could potentially reduce antibiotic prescriptions, decrease infection rates, and improve outcomes through early detection.[43]
Other players in the CLIA market
Other entities are beginning to focus on the CLIA market as well. Take AmericanBio, a custom reagent manufacturer that announced in October 2014 that it was implementing a "CLIA Grade product line and CLIA Grade Custom Manufacturing Services," helping device manufacturers sort through "regulatory framework, validation needs, consistency, and quality driven metrics that will support their diagnostic tool," both traditional and molecular.[46] Additionally, seminars and webinars on getting medical devices CLIA-waived are appearing from market research companies like Research and Markets and government agencies like the National Institutes of Health.[47][48] And niche businesses like Precision for Medicine are popping up, offering specialty regulatory, device, and test development services for the CLIA market.[49]
Side-effects of cheap and easy testing
The CLIA market, however, is not without its warts. One of the potential side-effects of cheap and easy testing in the physician office is the occasional desire to monetize it, particularly when Medicare reimbursement for a particular set of tests is quite lucrative. While in the U.S. the profit-driven trend of health care has caused many to debate further changes, in truth physicians still must be concerned with at least meeting operating costs.[50] However, some physicians have been more opportunistic, particularly in the field of urine drug testing. A 2012 article in the Journal of Pain & Palliative Care Pharmacotherapy titled "Profit-Driven Drug Testing" showed urine drug screens for both waived and non-waived tests reimbursed by Medicare increased by 4,537 percent from 2000 to 2009. Even worse, "the total number of CLIA-waived drug tests (CPT Code 80101QW) paid for by Medicare and conducted at physicians’ offices increased approximately 3,172,910 percent; with 101 tests conducted in 2000 and 3,204,740 in 2009."[51] This sudden increase of reimbursements came in part because physicians could bill Medicare per panel, meaning an 11-panel urine drug screen could be billed 11 times. CMS amended their rules in 2010 to prevent this type of unintended billing behavior, making drug testing less lucrative in general, especially for the POL.[51]
Yet some labs with a CLIA certificate of compliance or accreditation to handle moderate to advanced tests would continue to skirt the issue by moving to advanced mass spectrometry urine drug tests (qualitative) due to Medicare guidelines that encourage doctors to test patients using pain medicines to ensure their proper usage. In late 2014, The Wall Street Journal reported that Medicare was spending $445 million on 22 advanced drugs-of-abuse tests in 2012, up by more than 1,400 percent from 2007. With separate tests for each substance screened, an incentive remained for laboratories and physicians to abuse moderate- to advanced-level urine drug testing.[52]
In The Practical Guide to the U.S. Physician Office Laboratory, four economic considerations were outlined: billing, insurance reimbursements, profitability/sustainability, and return on investment (ROI). In truth, all these considerations are closely related to each other, with the goal of at least meeting operating costs while providing quality care to patients. However, plenty of challenges must be navigated along the way, from meeting state and federal regulatory requirements to billing properly. For the POL in particular the practice must decide which tests to offer, finding balance between the most commonly ordered IVD tests — such as dipstick urinalysis, complete blood counts, and prothrombin time[53] — and those that will potentially see rapid revenue growth, including anemia tests, chronic inflammation tests, and the glycated hemoglobin (HbA1c) diabetic test.[54]
Another area POL operators must keep a close eye on is healthcare reform and reimbursement changes. The aforementioned 2010 CMS changes to urine drug screening compensation is one of many examples of how changing regulations and reimbursements can affect a POL's bottom line. The economics of data management, which tools to use and what data to save represent more considerations for the POL. "To improve clinical lab profitability in today's healthcare environment, it is essential for any practice to establish an ongoing process to produce data relevant to the management of its patient base," Medical Source, Inc. CEO Keith LaBonte said in 2011, also noting the importance of identifying relevant data and implementing effective processes for staff to collect and organize those data in data management systems.[55]
One recent issue that economically threatens the U.S. POL's bottom line relates to the Protecting Access to Medicare Act passed in April 2014. Though its original purpose was to delay Medicare payment cuts to physicians until March 2015, Medicare cuts targeting the clinical laboratory fee schedule starting on January 1, 2017 potentially threaten small laboratories, including POLs. CMS will be switching to market-based rate changes that researchers like Kalorama Information and organizations like the National Independent Laboratory Association (NILA) and the American Association for Clinical Chemistry (AACC) believe will adversely affect small laboratories.[56][28][57]
"Most concerning to NILA and the small labs it represents is the prospect of significant drops in prices to routine tests. Community and regional labs are especially sensitive to price pressures since they often serve vulnerable populations in niche markets that national labs do not, such as nursing homes or homebound patients who require phlebotomists to visit them. This leaves community labs little means to cope with declining reimbursement..."[57] - Bill Malone, Clinical Laboratory News managing editor
"[R]outine tests are likely to see the sharpest reductions in reimbursement with the enactment of the Act’s market-based pricing reform. Routine tests performed at the point of care (POC) or in a physician office laboratory (POL) are most vulnerable, as the cost of the test is often higher without the scale and efficiencies of a core lab environment. Non-automated tests or routine, waived manual tests with a unique code are unlikely to see price erosion on the scale of those largely performed on automated instruments in higher volume private and hospital labs. Benchtop analyzers performing low volume automated POC testing in clinics and offices could represent an increasingly poor proposition for physician offices and other POC testers as market-averaged reimbursement rates slide towards the per-test costs achieved at large labs."[56] - Kalorama Information, a market research company
Data management
The role of the laboratory is shifting by internal forces like the adoption of new technology as well as external ones such as consumerism, information availability, and the development of complicated data streams. Laboratory professionals are moving to a role that places them in the center of the data stream. As such, effective data collection and management is becoming more important than ever. This requires not only quality tools but also staff-friendly processes that can easily be followed and updated.
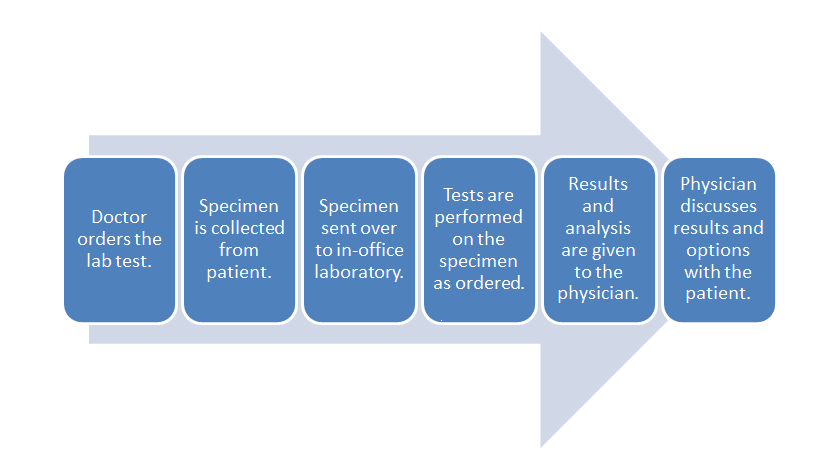
- POL workflow:
The above diagram shows the typical workflow for POL data management. While managing this workflow is important, the data associated with it go beyond ordinary practice function; these data can be used to assist with tracking population health for the patients or be combined with financial data such as billing or spending on supplies.
Other data streams may be generated outside this typical workflow as well. Meaningful Use Stage 3 will eventually require EHRs to accept patient-generated data. These data can come from tracking tools like Fitbits or from glucometers used by the patient.[58] Such data can aid the physician with diagnosis by giving them more data points to examine, but this may also impact the data management methods of the practice.
This area is a future frontier in the quest to use technology as a means of improving outcomes while driving costs down. The popularity of these patient devices and the trend towards using technology for healthcare purposes is drawing physician interest in using such devices for expanded monitoring of patients, with indicators supporting this trend on the development side.[58] The Scanadu Scanaflo, which "measures up to 12 reagents" as well as pH, represents another such device. Scanaflo is still in development, but it will work with a smartphone app and allow patients to monitor many areas of their health from home.[27] Results can be stored and interpreted via the app, and that data can eventually make its way into a physician's Stage 3-compliant EHR. (An interesting video about generating data at home with Scanadu devices can be viewed here.)
Data management tools
Laboratory data management for a POL is generally done via a laboratory information system (LIS), a software system that records, manages, and stores data for clinical laboratories. The LIS is usually able to connect to laboratory instruments, track orders, and record and store results. A modern LIS is also capable of integrating with an electronic health record (EHR) — a digital patient record capable of being shared across different health care settings — to allow the results to be stored in the complete patient record. This is an easier task for the POL, but if the results are coming in from an outside laboratory, an online healthcare marketplace service such as Health Gorilla (formerly Informedika) can be of great assistance.
Other tools for connecting the lab with the physician office are popping up too. Clinical information exchange systems are being designed to optimize workflows using application programming interfaces (APIs) and web services technology to connect systems.[59] Computerized provider order entry (CPOE) systems are also increasingly being used. In many cases these systems are used for entering drug orders, but these systems can also be used to enter laboratory testing orders. This offers an opportunity for laboratory professionals to assist physicians with choosing the appropriate test.[60]
When done well, laboratory data management can allow physician offices to track data for multiple business processes as well as patient care. This is made easier when software systems are interfaced and the staff is trained in their use. As such, laboratory personnel should be part of the data management system decision making processes, especially given the introduction of patient-generated laboratory data. This also provides an opportunity for laboratory directors to get involved, as they are the ones ultimately responsible for compliance with regulatory issues.
See the Data Management section of this guide for more information.
Data management challenges
As mentioned previously, changes to HIPPA rules now require laboratories to give results to the patient within 30 days of a written request by patient or authorized agent. This complicates the process of managing laboratory data, which should be kept in both the LIS and the patient EHR. Rapid data transfer to these systems can be facilitated through an interface with lab instruments, extracting and storing the results. Some POL instruments can do this directly through an interface while others (a point-of-care glucometer, for example) may need to have its data entered in manually.
Another challenge for physicians is deciding on a certified EHR. Slightly more than 1,400 Meaningful Use Stage 1 certified EHRs (about 72 percent of all certified EHRs) had not become Stage 2 certified by the end of 2014. This puts many laboratories in a difficult position because they must create new interfaces for physicians forced to replace their previous EHR. However, laboratory operators have seen all kinds of EHRs and are in a unique position to advise physicians on how to best replace their EHR. This is an advantage for the POL: one can buy a LIS and an EHR at the same time and get opinions from other laboratories about how well they interface.[61]
However, with Meaningful Use Stage 3 requirements due to take effect in 2016, and seeing as how more than 70 percent of EHRs are not Stage 2-compliant, how many options will actually be ready to accept patient-generated data via Stage 3 compliancy?
CLIA regulations hold laboratory directors responsible for compliance with data reporting EHR requirements. In-house laboratories such as the POL are not impacted by some of the challenges regarding CLIA requirements; however, they can still be impacted by the requirements to collect data from multiple sources and put that data into the patient record.[62] As most POLs are operating on a CLIA certificate of waiver and the requirements for the laboratory director are minimal, an air of complacency can evolve in the POL environment. However, a POL's laboratory director must focus on being proactively involved with data collection and management functions as well as the EHR and LIS selection and familiarization process.
References
- ↑ 1.0 1.1 1.2 1.3 1.4 Centers for Medicare and Medicaid Services, Division of Laboratory Services (July 2015). "Enrollment, CLIA exempt states, and certification of accreditation by organization" (PDF). http://www.cms.gov/Regulations-and-Guidance/Legislation/CLIA/Downloads/statupda.pdf. Retrieved 01 December 2015.
- ↑ 2.0 2.1 2.2 2.3 2.4 2.5 2.6 2.7 Garrels, Marti; Oatis, Carol S. (2014). Laboratory and Diagnostic Testing in Ambulatory Care: A Guide for Healthcare Professionals (3rd ed.). Elsevier Health Sciences. pp. 368. ISBN 9780323292368. https://books.google.com/books?id=LM9sBQAAQBAJ. Retrieved 18 April 2015.
- ↑ "Careers in Pathology and Medical Laboratory Science" (PDF). American Society for Clinical Pathology. http://www.ascp.org/pdf/CareerBooklet.aspx. Retrieved 18 April 2015.
- ↑ "Laboratory Safety Standards". American National Standards Institute. 2015. http://webstore.ansi.org/laboratory_safety/. Retrieved 18 April 2015.
- ↑ 5.0 5.1 Centers for Disease Control and Prevention (31 May 2013). "Clinical Laboratory Improvement Amendments (CLIA): Test complexities". http://wwwn.cdc.gov/clia/Resources/TestComplexities.aspx. Retrieved 18 April 2015.
Cite error: Invalid
<ref>tag; name "CDCTestCom" defined multiple times with different content - ↑ "CLIA - Clinical Laboratory Improvement Amendments - Currently Waived Analytes". U.S. Food and Drug Administration. 13 April 2015. http://www.accessdata.fda.gov/scripts/cdrh/cfdocs/cfClia/analyteswaived.cfm. Retrieved 18 April 2015.
- ↑ Kulczycki, Michael (1 April 2014). "Focusing on Provider-Performed Microscopy Procedure Requirements for Ambulatory Health Care". Ambulatory Buzz. The Joint Commission. http://www.jointcommission.org/musingsambulatory_patient_safety/focusing_provider_microscopy_procedure_req_ambulatory_health_care/. Retrieved 18 April 2015.
- ↑ Taylor, Jean M.; Stein, Gary C.; Weinberg, Sandy (2002). "Chapter 1: Historical Perspective". Good Laboratory Practice Regulations (3rd ed.). CRC Press. pp. 1–24. ISBN 9780203911082. https://books.google.com/books?id=50P7CAAAQBAJ&pg=PA1. Retrieved 19 May 2015.
- ↑ Seiler, Jürg P. (2006). "Chapter 1: What Is Good Laboratory Practice All About?". Good Laboratory Practice (2nd ed.). Springer Science & Business Media. pp. 1–58. ISBN 9783540282341. https://books.google.com/books?id=Hhj1sDFIlOYC&pg=PA1. Retrieved 19 May 2015.
- ↑ "Public Law 90-174" (PDF). United States Statutes at Large, Volume 81. 1967. http://www.gpo.gov/fdsys/pkg/STATUTE-81/pdf/STATUTE-81-Pg533.pdf. Retrieved 24 March 2014.
- ↑ 11.0 11.1 "Public Law 100-578" (PDF). United States Statutes at Large, Volume 102. 1988. http://www.gpo.gov/fdsys/pkg/STATUTE-102/pdf/STATUTE-102-Pg2903.pdf. Retrieved 24 March 2014.
- ↑ 12.0 12.1 12.2 Cox, Phyllis; Wilken, Danielle (2010). "Chapter 1: Safety in the Laboratory". Palko's Medical Laboratory Procedures (3rd ed.). McGraw-Hill Education. pp. 1–23. ISBN 9780073401959. https://books.google.com/books?id=6uWWPQAACAAJ. Retrieved 18 April 2015.
- ↑ "Examples of Common Laboratory Chemicals and their Hazard Class". National Institutes of Health, Office of Management. 27 November 2012. http://orf.od.nih.gov/EnvironmentalProtection/WasteDisposal/Pages/Examples+of+Common+Laboratory+ChemicalsandtheirHazardClass.aspx. Retrieved 18 April 2015.
- ↑ "CLIA Program and HIPAA Privacy Rule; Patients' Access to Test Reports" (PDF). Federal Register 79 (25): 7290–7316. 6 February 2014. http://www.gpo.gov/fdsys/pkg/FR-2014-02-06/pdf/2014-02280.pdf. Retrieved 13 April 2015.
- ↑ Hughes, D.; Cammarata, B. (16 January 2014). "Clinical labs under ACA: Challenge and opportunity". Law360. http://www.law360.com/articles/500623/clinical-labs-under-aca-challenge-and-opportunity. Retrieved 18 April 2015.
- ↑ "CLIA Categorization Criteria". U.S. Food and Drug Administration. 6 March 2014. http://www.fda.gov/MedicalDevices/DeviceRegulationandGuidance/IVDRegulatoryAssistance/ucm124208.htm. Retrieved 23 March 2014.
- ↑ "Clinical Laboratory Improvement Amendments (CLIA) - CLIA Waived Tests". Centers for Disease Control and Prevention. 14 March 2014. http://wwwn.cdc.gov/clia/Resources/WaivedTests/default.aspx. Retrieved 23 March 2014.
- ↑ "Certificate of Waiver Laboratory Project". Centers for Medicare and Medicaid Services. 27 February 2014. https://www.cms.gov/Regulations-and-Guidance/Legislation/CLIA/Certificate_of_-Waiver_Laboratory_Project.html. Retrieved 19 May 2015.
- ↑ 19.0 19.1 "How to Apply for a CLIA Certificate, Including International Laboratories". Centers for Medicare and Medicaid Services. 30 April 2012. https://www.cms.gov/Regulations-and-Guidance/Legislation/CLIA/How_to_Apply_for_a_CLIA_Certificate_International_Laboratories.html. Retrieved 19 May 2015.
- ↑ 20.0 20.1 "Point Of Care Testing". College of American Pathologists. September 2013. http://www.cap.org/apps//cap.portal?_nfpb=true&cntvwrPtlt_actionOverride=%2Fportlets%2FcontentViewer%2Fshow&_windowLabel=cntvwrPtlt&cntvwrPtlt{actionForm.contentReference}=policies%2Fpolicy_appII.html. Retrieved 18 April 2015.
- ↑ Kiechle, Frederick L.Main, Rhonda Ingram (2002). The Hitchhiker's Guide to Improving Efficiency in the Clinical Laboratory. American Association for Clinical Chemistry. pp. 132. ISBN 9781890883720. https://books.google.com/books?id=ud55aVHAiTQC. Retrieved 13 April 2015.
- ↑ "Point-of-Care Diagnostic Testing". Research Portfolio Online Reporting Tools. National Institutes of Health. 29 March 2013. http://report.nih.gov/nihfactsheets/ViewFactSheet.aspx?csid=112. Retrieved 18 April 2015.
- ↑ 23.0 23.1 "Waived and Provider Performed Microscopy (PPM) Tests". American Academy of Family Physicians. http://www.aafp.org/practice-management/regulatory/clia/tests.html. Retrieved 19 May 2015.
- ↑ "Provider-performed Microscopy Procedures" (PDF). Centers for Medicare and Medicaid Services. http://www.cms.gov/Regulations-and-Guidance/Legislation/CLIA/downloads/ppmplist.pdf. Retrieved 19 May 2015.
- ↑ "Integrating Laboratories Into the PCMH Model of Health Care Delivery: A COLA White Paper" (PDF). 2014. p. 3–4. http://www.cola.org/wp-content/uploads/2014/10/COLA_14194-PCMH-White-paper-V3-FINAL.pdf. Retrieved 14 April 2015.
- ↑ Goyal, Nidhi (4 April 2015). "VeinViewer Means No More Poking People Relentlessly to Locate Veins". Industry Tap. http://www.industrytap.com/veinviewer-means-no-poking-people-relentlessly-locate-veins/27706. Retrieved 14 April 2015.
- ↑ 27.0 27.1 Buhr, Sarah (18 February 2015). "Scanadu’s New Pee Stick Puts The Medical Lab On Your Smartphone". Tech Crunch. AOL, Inc. http://techcrunch.com/2015/02/18/scanadus-new-pee-stick-puts-the-medical-lab-on-your-smartphone/. Retrieved 14 April 2015.
- ↑ 28.0 28.1 28.2 Park, Richard (13 October 2014). "Examining the Physician Office Lab Market: Growth and Reimbursement". Medical Design Technology. Advantage Business Media. http://www.mdtmag.com/blogs/2014/10/examining-physician-office-lab-market-growth-and-reimbursement. Retrieved 01 June 2015.
- ↑ "How and Where IVD Will Find Growth in the Global POL Market – Part 2". Kalorama Information. November 2014. http://www.kaloramainformation.com/article/2014-11/How-and-Where-IVD-Will-Find-Growth-Global-POL-Market-%E2%80%93-Part-2. Retrieved 07 July 2015.
- ↑ Park, Richard (29 September 2014). "Examining the Physician Office Lab Market: CLIA and Technology". Medical Design Technology. Advantage Business Media. http://www.mdtmag.com/blogs/2014/09/examining-physician-office-lab-market-clia-and-technology. Retrieved 01 June 2015.
- ↑ 31.0 31.1 "Administrative Procedures for CLIA Categorization: Guidance for Industry and Food and Drug Administration Staff" (PDF). U.S. Department of Health and Human Services. 12 March 2014. http://www.fda.gov/downloads/MedicalDevices/DeviceRegulationandGuidance/GuidanceDocuments/ucm070889.pdf. Retrieved 01 June 2015.
- ↑ 32.0 32.1 32.2 Wirt, Tammy (24 March 2014). "NWS HHS FDA CRDH" (PDF). U.S. Food and Drug Administration. http://www.fda.gov/downloads/Training/CDRHLearn/UCM390761.pdf. Retrieved 01 June 2015.
- ↑ "Fact Sheet: Medical Device User Fee Amendments of 2012". U.S. Food and Drug Administration. 3 August 2012. http://www.fda.gov/RegulatoryInformation/Legislation/FederalFoodDrugandCosmeticActFDCAct/SignificantAmendmentstotheFDCAct/FDASIA/ucm313695.htm. Retrieved 01 June 2015.
- ↑ Mullen, Allyson B. (19 March 2014). "FDA Issues Revised Final Guidance Regarding Administrative Procedures for CLIA Categorization". FDA Law Blog. Hyman, Phelps & McNamara, P.C. http://www.fdalawblog.net/fda_law_blog_hyman_phelps/2014/03/fda-issues-revised-final-guidance-regarding-administrative-procedures-for-clia-categorization.html. Retrieved 01 June 2015.
- ↑ Rath, Prakash (5 March 2014). "Administrative Changes to FDA’s CLIA Categorization Program" (PDF). U.S. Food and Drug Administration. http://ftp.cdc.gov/pub/CLIAC_meeting_presentations/pdf/Addenda/cliac0314/04_Rath_Admin%20Changes%20to%20FDA%27s%20CLIA%20Program.pdf. Retrieved 01 June 2015.
- ↑ "CLIA Waiver by Application". U.S. Food and Drug Administration. 26 March 2015. http://www.fda.gov/MedicalDevices/DeviceRegulationandGuidance/IVDRegulatoryAssistance/ucm393233.htm. Retrieved 01 June 2015.
- ↑ "Quidel Receives Simultaneous FDA Clearance And CLIA Waiver For Its Sofia® Strep A+ Fluorescent Immunoassay (FIA) Via The FDA's New Dual Submission Program". Med Device Online. VertMarkets, Inc. 17 December 2014. http://www.meddeviceonline.com/doc/quidel-receives-simultaneous-fda-clearance-and-clia-waiver-0001. Retrieved 01 June 2015.
- ↑ "Trinity Biotech Announces CLIA Waiver of Rapid Syphilis Test". GlobeNewswire, Inc. 16 December 2014. http://globenewswire.com/news-release/2014/12/16/691813/10112606/en/Trinity-Biotech-Announces-CLIA-Waiver-of-Rapid-Syphilis-Test.html. Retrieved 26 May 2015.
- ↑ "HIV testing - prevalent CLIA waived tests". Percepta Associates, Inc. 12 March 2015. http://www.perceptaassociates.com/hiv-testing-clia-waived-tests/. Retrieved 26 May 2015.
- ↑ "Trinity Biotech Receives CLIA Waiver for Uni-Gold(TM) Recombigen(R) HIV Test". PR Newswire Association LLC. 10 November 2014. http://www.prnewswire.com/news-releases/trinity-biotech-receives-clia-waiver-for-uni-goldtm-recombigenr-hiv-test-75323487.html. Retrieved 26 May 2015.
- ↑ 41.0 41.1 41.2 Johnson, Madeleine (26 April 2015). "Cepheid Sees 'Significant Opportunity' in Menu Expansion, CLIA Market". GenomeWeb. Genomeweb LLC. https://www.genomeweb.com/business-news/cepheid-sees-significant-opportunity-menu-expansion-clia-market. Retrieved 21 May 2015.
- ↑ 42.0 42.1 Johnson, Madeleine (19 June 2014). "With FDA-Cleared Flu Test, Alere Launches Isothermal MDx Platform for US Clinical Market". GenomeWeb. Genomeweb LLC. https://www.genomeweb.com/pcrsample-prep/fda-cleared-flu-test-alere-launches-isothermal-mdx-platform-us-clinical-market. Retrieved 21 May 2015.
- ↑ 43.0 43.1 43.2 Seiffert, Don (12 January 2015). "FDA waiver of Alere's flu test poses threat to market leader Cepheid". Boston Business Journal. American City Business Journals. http://www.bizjournals.com/boston/blog/bioflash/2015/01/fda-waiver-of-aleres-flu-test-poses-threat-to.html. Retrieved 21 May 2015.
- ↑ Johnson, Madeleine (30 April 2015). "Q&A: BioMérieux's Christine Ginocchio Chats About Her Clinical Lab Career Arc, Syndromic PCR Panels". GenomeWeb. Genomeweb LLC. https://www.genomeweb.com/pcr/qa-biom-rieuxs-christine-ginocchio-chats-about-her-clinical-lab-career-arc-syndromic-pcr-panels. Retrieved 26 May 2015.
- ↑ 45.0 45.1 Johnson, Madeleine (12 January 2015). "With CLIA Waiver and Widespread Flu, Alere Ramps Up Molecular Test Production". GenomeWeb. Genomeweb LLC. https://www.genomeweb.com/pcr/clia-waiver-and-widespread-flu-alere-ramps-molecular-test-production. Retrieved 21 May 2015.
- ↑ "AmericanBio expands product offerings, introduces exclusive CLIA Grade product line". AmericanBio, Inc. 17 October 2014. https://www.americanbio.com/news-events/americanbio-expands-product-offerings-introduces-exclusive-clia-grade-product-line1. Retrieved 27 May 2015.
- ↑ "How to get a CLIA Waiver for your Medical Device: One and a Half Day In-person Seminar 2015 (Newark, NJ)". Research and Markets. May 2015. http://www.researchandmarkets.com/reports/3215400/how-to-get-a-clia-waiver-for-your-medical-device. Retrieved 27 May 2015.
- ↑ ""CLIA Waivers: The What, The Why, and The How" Webinar". National Institutes of Health. 15 April 2015. http://www.nibib.nih.gov/news-events/meetings-events/clia-waivers-what-why-and-how-webinar. Retrieved 27 May 2015.
- ↑ "Regulatory Solutions". Precision for Medicine. http://www.precisionformedicine.com/regulatory-solutions/. Retrieved 27 May 2015.
- ↑ Ubel, Peter (12 February 2014). "Is The Profit Motive Ruining American Healthcare?". Forbes.com. Forbes, Inc. http://www.forbes.com/sites/peterubel/2014/02/12/is-the-profit-motive-ruining-american-healthcare/. Retrieved 27 May 2015.
- ↑ 51.0 51.1 Collen, Mark (2012). "Profit-Driven Drug Testing". Journal of Pain & Palliative Care Pharmacotherapy (26): 13–17. doi:10.3109/15360288.2011.650358. http://www.academia.edu/7840929/Profit-driven_drug_testing. Retrieved 27 May 2015.
- ↑ Weaver, Christopher; Matthews, Anna-Wilde (10 November 2014). "Doctors Cash In on Drug Tests for Seniors, and Medicare Pays the Bill". The Wall Street Journal. Dow Jones & Company, Inc. http://www.wsj.com/articles/doctors-cash-in-on-drug-tests-for-seniors-and-medicare-pays-the-bill-1415676782. Retrieved 01 June 2015.
- ↑ "Top 10 Tests In Physician Office Revealed". Kalorama Information. 10 December 2014. http://www.kaloramainformation.com/about/release.asp?id=3686. Retrieved 05 June 2015.
- ↑ "Report: Five Fastest-Growing Tests in Physician Office Labs". PR Newswire. 18 December 2014. http://www.prnewswire.com/news-releases/report-five-fastest-growing-tests-in-physician-office-labs-300010866.html. Retrieved 05 June 2015.
- ↑ 56.0 56.1 "Recapping the 'Doc Fix' Act's Impacts on Medicare Lab Reimbursement". Kalorama Information. June 2014. http://www.kaloramainformation.com/article/2014-06/Recapping-Doc-Fix-Acts-Impacts-Medicare-Lab-Reimbursement. Retrieved 02 June 2015.
- ↑ 57.0 57.1 Malone, Bill (1 June 2014). "A New Era for Lab Reimbursement". Clinical Laboratory News. American Association for Clinical Chemistry. https://www.aacc.org/publications/cln/articles/2014/june/lab-reimbursement. Retrieved 02 June 2015.
- ↑ 58.0 58.1 McLeod, Pamela Scherer (19 March 2015). "Physicians Use Fitness Trackers to Monitor Patients in Real-time, Even as Developers Work to Incorporate Medical Laboratory Tests into the Devices". Dark Daily. Dark Intelligence Group, Inc. http://www.darkdaily.com/physicians-use-fitness-trackers-to-monitor-patients-in-real-time-even-as-developers-work-to-incorporate-medical-laboratory-tests-into-the-devices-528. Retrieved 14 April 2015.
- ↑ Michel, Robert (30 March 2015). "How Medical Laboratories Help Physicians Overcome the Failure of Many EHR Systems to Support Effective Lab Test Ordering and Lab Result Reporting". DarkDaily.com. Dark Intelligence Group, Inc. http://www.darkdaily.com/how-medical-laboratories-help-physicians-overcome-the-failure-of-many-ehr-systems-to-support-effective-lab-test-ordering-and-lab-result-reporting-330.
- ↑ Sinard, John (2006). Practical Pathology Informatics: Demystifying Informatics for the Practicing Anatomic Pathologist. Springer Science & Business Media. pp. 412. ISBN 9780387280585. https://books.google.com/books?id=WerUyK618fcC. Retrieved 14 April 2015.
- ↑ Michel, Robert (19 March 2015). "Most Clinical Laboratories and Pathology Groups Unprepared to Help Client Physicians Meet Meaningful Use Stage 2 Criteria". Dark Daily. Dark Intelligence Group, Inc. http://www.darkdaily.com/most-clinical-laboratories-and-pathology-groups-unprepared-to-help-client-physicians-meet-meaningful-use-stage-2-criteria. Retrieved 14 April 2015.
- ↑ Henricks, Walter H. (18 March 2015). "Accreditation and Regulatory Implications of Electronic Health Records for Laboratory Reporting". InsuranceNewsNet.com, Inc. http://insurancenewsnet.com/oarticle/2015/03/18/accreditation-and-regulatory-implications-of-electronic-health-records-for-labor-a-606123.html. Retrieved 14 April 2015.