Journal:Laboratory automation, informatics, and artificial intelligence: Current and future perspectives in clinical microbiology
| Full article title | Laboratory automation, informatics, and artificial intelligence: Current and future perspectives in clinical microbiology |
|---|---|
| Journal | Frontiers in Cellular and Infection Microbiology |
| Author(s) | Mencacci, Antonella; De Socio, Guiseppe V.; Pirelli, Eleonora; Bondi, Paola; Cenci, Elio |
| Author affiliation(s) | University of Perugia, Perugia General Hospital |
| Primary contact | Email: antonella at mencacci at unipg dot it |
| Editors | Blasi, Elisabetta |
| Year published | 2023 |
| Volume and issue | 13 |
| Article # | 1188684 |
| DOI | 10.3389/fcimb.2023.1188684 |
| ISSN | 2235-2988 |
| Distribution license | Creative Commons Attribution 4.0 International |
| Website | https://www.frontiersin.org/articles/10.3389/fcimb.2023.1188684/full |
| Download | https://www.frontiersin.org/articles/10.3389/fcimb.2023.1188684/pdf (PDF) |
Abstract
Clinical diagnostic laboratories produce one product—information—and for this to be valuable, the information must be clinically relevant, accurate, and timely. Although diagnostic information can clearly improve patient outcomes and decrease healthcare costs, technological challenges and laboratory workflow practices affect the timeliness and clinical value of diagnostics. This article will examine how prioritizing laboratory practices in a patient-oriented approach can be used to optimize technology advances for improved patient care.
Keywords: laboratory automation, artificial intelligence, informatics, laboratory workflow, Kiestra, WASPLab
Introduction
Patterns of infectious diseases have changed dramatically: patients are frequently immunocompromised and often have complicating comorbidities; infections with multi-drug-resistant organisms (MDRO) are a global problem; and new antibiotics are available, but it is mandatory to preserve their efficacy. It is estimated that at least 700,000 people die worldwide every year with infections caused by MDRO, and it is predicted that by 2050, 10 million deaths might occur due to these organisms.[1] Administration of rapid, broad-spectrum empiric therapy is essential to improve patient outcome[2], but this is often inappropriate.[3][4] For example, meta-analysis assessing the impact of antibiotic therapy on Gram-negative sepsis showed that inappropriate therapy was associated with 3.3-fold increased risk of mortality, longer hospitalization, and higher costs.[5] Thus, rapid, accurate diagnostics are critical for the selection of the most appropriate therapy.
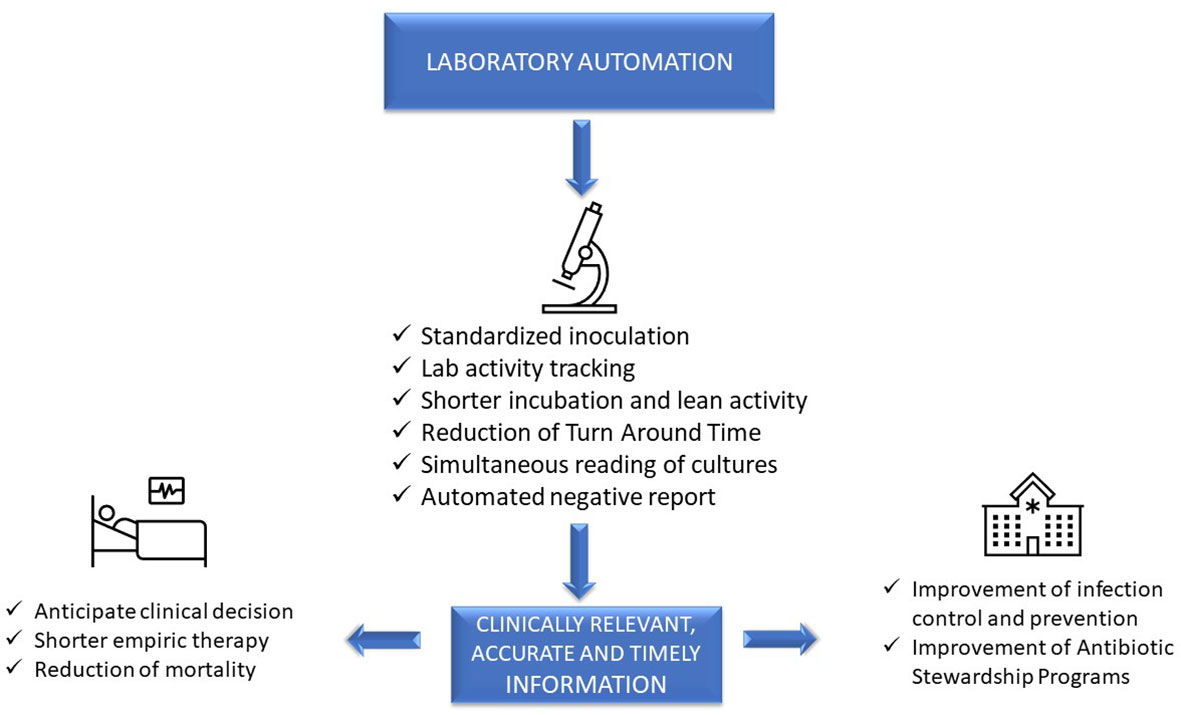
Advanced, sophisticated technologies such as mass spectrometry and molecular diagnostics are rapidly changing our ability to diagnose infections[6], although they should be viewed as complementary to traditional growth-based diagnostics. Laboratory automation and intelligent applications of of informatics also have a transformative impact of microbiology diagnostics. These tools have the potential to accelerate clinical decision-making and positively impact the management of infections, improve patient outcome, and facilitate diagnostic and antimicrobial stewardship (AS) programs.[7] However, it is a challenge for clinical microbiologists to implement these technologies because it requires changing well-established workflow practices. This paper will focus on the impact of automation and informatics combined with workflow changes on laboratory, patient, and hospital management (Figure 1).
|
Impact on laboratory management
In clinical microbiology, the term “total laboratory automation” (TLA) is used to describe the automation of the entire diagnostic workflow, from inoculation of the agar plates to incubation, reading of culture results, identification (ID), and antimicrobial susceptibility testing (AST). All these steps in a conventional laboratory are performed manually, usually according to a sample-centered approach. At present, two laboratory automation systems are available: the BD Kiestra system (Becton Dickinson, Sparks, MD) and the WASPLab system (Copan Diagnostics, Murrieta, CA).[8] We discuss these systems within the context of this workflow and then address other laboratory automation tools, as well artificial intelligence (AI).
Inoculation
Quality and precision of inoculation are improved by automation. Instruments work in a standardized and consistent mode, not achievable with a manual procedure, and independent of operator variability. Indeed, laboratory automation allows better isolation of colonies compared to manual inoculation, with decreased need of subcultures for follow-up work, mainly AST, resulting in a more rapid report.[9][10] It was found that WASP automated streaking of urines using a sterile loop was superior to manual streaking, yielding a higher number of single colonies and of detected morphologies, species, and pathogens.[11] The BD Kiestra system, based on a rolling magnetic bead streaking technology, has been shown to improve the accuracy of quantitative culture results and the recovery of discrete colonies from polymicrobial samples, compared to manual and automated WASP streaking.[9][12] This implies a reduction of bacterial subcultures to perform ID and AST, thus shortening time to results, as evidenced for urines[13] and both methicillin-resistant Staphylococcus aureus (MRSA) and carbapenem-resistant Enterobacterales screening samples.[14]
Incubation
Closed incubators with digital imaging of cultures allow more rapid growth than conventional incubators that are opened frequently throughout the day. Moreover, in TLA, plates are fully tracked as long as they stay within the system, so that it is possible to define by hours and minutes incubation times and plate examination, in contrast with the traditional system in which incubation times are defined in days. Burckhardt et al. showed that first growth of MRSA, multi-drug-resistant (MDR) Gram-negative bacteria, and vancomycin-resistant enterococci (VRE) on selective chromogenic plates was visible as early as after four hours of inoculation, although the bacterial mass was not sufficient for follow-up work.[15] Also, growth of Escherichia coli, Pseudomonas aeruginosa, Enterococcus faecalis, and S. aureus on chromogenic plates was three to four hours faster in the automated system than in the classic system.[16] Implementation of BD Kiestra TLA significantly improved turnaround times (TAT) for positive and negative urine cultures.[17] Similarly, WASPLab automation enabled a reduction of the culture reading time for different specimens without affecting performances.[18] However, minimum incubation times for each type of specimen, for a timely and accurate positive or negative report, are not yet defined, and additional studies are needed.
Reading
The Kiestra laboratory automation system, through a real-time dashboard, times tasks as they are scheduled. Thus, each technician perfectly knows when the culture plates will be ready for reading and when follow-up work can be performed. This strongly facilitates laboratory workflow management, avoiding wasted time and allowing results to be delivered to the clinician as soon as possible. In addition, while in the classical system plates are read one by one, digital reading allows simultaneous viewing of all the plate images from the same sample, and even of different samples from the same patient. This greatly facilitates and speeds up the interpretation of culture results, either for monomicrobial or polymicrobial infections.
ID and AST
The implementation of TLA in clinical microbiology has leveraged the advancement brought by matrix-assisted laser desorption/ionization time-of-flight mass spectrometry (MALDI-TOF/MS).[19][20] Furthermore, Copan’s TLA has recently integrated an automated device (Colibri) that can reproducibly prepare the MALDI target for microbial identification. A recent study conducted by Cherkaoui et al. established that the WASPLab coupled to MALDI-TOF/MS significantly reduces the TAT for positive blood cultures.[21] Similarly, the BD Kiestra IdentifA/SusceptA, a prototype for automatic colony picking, bacterial suspension preparation, MALDI-TOF target plates spotting, and Phoenix M50 AST panel preparation, exhibited high ID and AST performances.[22] In particular, the IdentifA showed excellent identification rates for Gram-negative bacteria, outperforming manual processing for Enterobacterales identification[22], but not for streptococci, coagulase-negative staphylococci (CoNS), and yeasts.[22]
Finally, an automated solution for disk diffusion AST was developed and integrated with the Copan WASPLab system. It prepares inoculum suspensions, inoculates culture media plates, dispenses appropriate antibiotic disks according to predefined panels, transports the plates to the incubators, takes digitalized images of the media plates, and measures and interprets the inhibition zones’ diameters. Cherkaoui et al.—evaluating 718 bacterial strains, including S. aureus, CoNS, E. faecalis, Enterococcus faecium, P. aeruginosa, and different species of Enterobacterales—found 99.1% overall categorical agreement between this automated AST and Vitek2.[23]
Artificial intelligence
The development of intelligent image analysis based on tailored algorithms designed on type of specimens and patient characteristics allows automated detection of microbial growth, release of negative samples, presumptive ID, and quantification of bacterial colonies. This represents a major innovation that has the potential to increase laboratory quality and productivity while reducing TAT.[13] Promising results have been obtained on urine samples, with a 97%–99% sensitivity and 85%–94% specificity by the BD Kiestra system.[15] By a different approach, the WASPLab Chromogenic Detection Module has developed automated categorization of agar plates as “negative” (i.e., sterile) or “non-negative,” comparing the same plate at time point zero to the plate after the established incubation time. With this system, an optimal diagnostic accuracy in MRSA[24], VRE[25], and carbapenemase-producing Enterobacteriaceae[26] detection has been observed.
Other functions of laboratory automation
Laboratory automation can greatly facilitate the implementation of an effective quality management system (QMS), which is required to ensure that reliable results are reported for patients. Laboratory automation systems automatically track and record all the useful information for quality control (QC): user credentials, media (e.g., lot number and expiration date), inoculation (e.g., volumes of samples, patterns, and times of streaking), incubation (e.g., atmosphere, temperature, and times) and imaging (e.g., digital images of plates and times) data.[27] Thus, the proper integration of laboratory automation with a laboratory information system (LIS) allows for complete traceability of the analytical process, from sample receipt to the final report.
Moreover, the possibility to access and review any taken image represents an invaluable tool from a diagnostic point of view (e.g., comparing morphology of colonies in recent and old samples from the same patient) and also for other activities such as monitoring laboratory quality, teaching, training, and discussing culture results with colleagues and clinicians.
Impact and possible improvements of laboratory automation
Impact on patient management
Clinical impact of an assay, a technology, or a modified workflow can be defined based on its added value for patient management. In the case of sepsis, this can be measured as time to targeted therapy and, hopefully, a decrease in the mortality rate. In manual processing laboratories, the activities are performed in batches, usually based on the type of sample and type of activity (e.g., inoculation, reading, ID, AST, technical validation, and clinical validation), and the results are usually delivered mostly during the morning hours. Indeed, a study evaluating the TAT for positive blood cultures (BC) in 13 US acute care hospitals demonstrated a significant discrepancy between times of BC collection and reporting laboratory test results. While only 25% of specimens were collected between 6:00 a.m. and 11:59 a.m., approximately 80% of laboratory ID and AST results were reported in this time interval.[28] This can have a negative impact on septic patient management, delaying clinical decision-making for optimal targeted therapy.
In contrast, in automated laboratories, the activity can be organized according to lean principles, creating a continuous “flow” and producing “just-in-time” results. De Socio et al. evaluated the impact of laboratory automation on septic patient management. Positive BC were processed by fully automatic inoculation on solid media and digital reading after eight hours of incubation, followed by ID and AST. The authors found that a reduction of time to report (TTR) of about one day led to a significant reduction of the duration of empirical therapy (from approximately 87 hours to approximately 55 hours) and of 30-day crude mortality rate (from 29.0% to 16.7%).[29]
Therefore, provided that the laboratory is open 24 hours a day, or taking advantage of telemedicine systems for clinical validation, laboratory automation has a potentially great impact on patient management. However, the success of such organization lies in the responsiveness of the medical teams, who should act upon the results soon after delivery by the laboratory.[30]
Impact on hospital management
Laboratory automation can improve the laboratory's ability to characterize MDRO and produce quality results, permitting a more standardized workflow, while leaving more time for laboratory staff to focus on second-level phenotypic and/or genotypic tests. Indeed, the large diffusion of MDRO and the expanding spectrum of resistance mechanisms among pathogens pointed out the limitations of commercial routine methods for susceptibility testing of selected antibiotics, increasing the demand for cumbersome and time-consuming reference methods. For example, in the case of MDRO Gram-negative isolates, colistin MIC should be determined by the broth microdilution method[31]; fosfomycin MIC, by the agar-dilution method[32]; and cefiderocol, a novel siderophore-conjugated cephalosporin, by the broth microdilution method using an iron-depleted cation-adjusted Mueller-Hinton broth.[33] Moreover, in the case of detection of uncommon resistance phenotypes, molecular methods, gene sequencing, or other next-generation sequencing (NGS) methods are often required.[34]
Accuracy is not sufficient per se for a result to be useful. Information must be given to clinicians or other healthcare providers (e.g., pharmacists and the patient’s primary care nurse) as quickly as possible. Timely reporting can affect hospital conditions in at least two ways: permitting the rapid control of the spread of MDRO (i.e., contact precautions, investigation of clusters of colonized/infected patients) and reducing the duration of broad-spectrum antibiotic therapy (i.e., positive results) or unnecessary empiric antibiotic therapy (i.e., negative results).
In a study proposing a cumulative antimicrobial resistance index as a tool to predict antimicrobial resistance (AR) trend in a hospital, a reversion of AR trend was observed in 2018, in comparison with the 2014–2017 period.[35] The authors speculate that this could have been a consequence of some changes in the management of infections in their hospital: (i) incubation of all BC within one hour from collection using satellite incubators, (ii) a significant reduction in TTR after the introduction of molecular technologies and laboratory automation, and (iii) an established close collaboration between infectious disease clinicians and clinical microbiologists.[35]
Finally, Culbreath et al. demonstrated that the implementation of TLA increased laboratory productivity by up to 90%, while reducing the cost per specimen by up to 47%, providing an excellent elaboration of the efficiencies and cost-savings that are achievable by implementation of full laboratory automation in the bacteriology laboratory.[36]
Possible improvements to laboratory automation systems
A detailed wish list of technical issues to be evaluated in order to improve the performance and workflow of laboratory automation systems has been recently published.[10] Here, we will focus on facts that, in our opinion, could affect laboratory, patient, and hospital management.
To facilitate the reading of the plates according to a patient-centered approach, it would be useful to view specimens’ Gram stains in the same screen of cultured plates. The images could also be shared with clinicians, improving clinician–microbiologist interplay. Further improvement can be made by automated microscopy systems, which can significantly reduce the workload of the technical staff.[37]
The availability of digital images lays the foundation for telebacteriology, intended as the use of digital imaging and file storage for on-screen reading and decision-making.[8] It makes it possible to geographically dissociate plate manipulation from reading and validation of the results. This could promote the microbiologist counseling activity and interaction with clinicians, as the images could be shared between consultants located at different sites. Also, it could support 24/7 laboratory activity, allowing the plates to be read outside the laboratory in a hub laboratory or even at home, with follow-up work performed in real time where the plates are incubated.
To make these technological innovations fully operational, a middleware information technology (IT) solution is needed to connect all the laboratory's instruments.[37]
Discussion
The main reason to introduce automation in a laboratory is to increase productivity in the face of limited budgets and personnel shortages. However, implementation of laboratory automation can represent an exceptional opportunity to change laboratory organization, improve quality, and reduce TTR, with a potential positive impact on laboratory, patient, and hospital management.
One of the most relevant innovations of laboratory automation regards the reading phase, with the possibility to read simultaneously all the plates inoculated from one of even more samples from the same patient. Moreover, taking advantage of informatics, it is also possible to view patient microbiological, hematological, and even clinical and therapeutic data while reading the plates. This patient-oriented approach provides meaningful clinical interpretation of results and decision-making.
By continuously tracing all the analytical steps, laboratory automation ensures that the microbiologist knows in real time the work to be carried out. This concept fully adheres to the so-called “lean” organization that, initially envisaged for industry[38]], is increasingly applied to healthcare processes. “Lean” means to do only valuable activities, without any delay, avoiding “waste” or unnecessary work. This implies a dramatic revolution in the mentality of microbiologists, transitioning from exclusively sample-centered laboratory work towards a more clinically oriented activity, shortening TTR and prioritizing diagnosis of time-dependent infections. Taking advantage of workflow optimization, a nearly 24 hour reduction in TTR has been observed for positive BC processed by laboratory automation, with a significant decrease of duration of empirical therapy and mortality.[29] Similar results were observed for urines[39] and nasal MRSA surveillance[40], as well as other specimen types.[13][17]
An AI algorithm to interpret culture results is another important tool applicable to laboratory automation: automated reporting of negative samples can be done without delay and further human assistance, such that clinicians can receive earlier results to rule out MDRO colonization or a urinary tract infection and reduce the need for patient isolation or antibiotic treatment.[20][24][25]
Outside laboratory automation, a variety of technologies are revolutionizing clinical microbiology. These include MALDI-TOF/MS[41], time-lapse microscopy for ID and phenotypic AST[42], molecular diagnostic tests and syndromic panels[6][43], and NGS.[44][45] All of them can significantly improve the diagnosis and therapy of infections, but as stated above, they are primarily complementary to culture-based methods.[6] Thus, in an advanced laboratory, the goal will be to implement the use of all these technologies in a coordinated and timely program of diagnostic stewardship (DS). For example, for active surveillance of MDRO, both molecular- and culture-based methods should be available in the laboratory.[46] Indeed, active surveillance of carbapenem-resistant Enterobacteriaceae can limit and prevent their spread and infections, which is crucially relevant to AS.[47] In high-risk patients, rapid molecular methods are more appropriate but cannot replace culture-based methods, as the latter can detect all types of carbapenem-resistant organisms, perform phenotypic susceptibility testing, and collect and store the isolates.[47]] An interesting algorithm—based on a multi-parametric score that takes into account clinical, microbiological, and biochemical parameters—has been recently proposed to establish patient priority, including information on infection or colonization by MDRO.[48] It is reasonable to think that by combining DS and AS programs with a strict collaboration between laboratory and clinicians, the impact of modern microbiology on the management of infection can progressively increase.
In this vein, rapid and effective communication from laboratory to wards and back is essential for optimal patient care. A recent study showed that many barriers exist, like verbal reporting of results, poorly integrated information systems, mutual lack of insight into each other’s area of expertise, and limited laboratory services.[49] Electronic reporting improves communication between microbiologists and clinical staff, but a type of alert system for the right physician (i.e., the treating clinician, an infectious diseases specialist, or a sepsis team member) to look up the data immediately should be integrated. Nevertheless, we believe that direct microbiologist/clinician interplay remains crucial for an optimal patient management: positive BC, detection of MDRO, isolation of alert organisms from sterile fluids, and acid-fast bacilli in respiratory samples must be immediately reported to someone who will act on the results.
Moreover, as microbiological methods become increasingly sophisticated, good clinical practice should be for the microbiologist to report the results with comments to facilitate the clinician’s interpretation of the significance of the data.[43] In our experience, after effective laboratory automation implementation, a closer relationship with clinicians is largely established, providing an opportunity to convey insight into microbiology and microbiological work processes to clinical staff. On the other hand, patients are increasingly complex and heterogeneous, and management of severe and MDRO infections is challenging, often requiring a multidisciplinary approach for optimal personalized diagnostics and therapy.[50] Therefore, to integrate DS with AS, microbiologists should broaden their knowledge of patient care by working closely with physicians.
Information from the microbiology laboratory is essential for the control and management of infections in a hospital. In particular, timely and accurate data on the antibiotic susceptibility profiles for pathogens isolated from different wards and on MDRO colonization/infection are the basis for setting up hospital infection control and AS programs, which can ultimately affect patient outcomes. Unfortunately, laboratories are not always able to provide timely information due to lack of specific expertise, personnel, user-friendly software, and optimized workflow practices. The implementation of laboratory automation and laboratory informatics can support integration into routine practice monitoring specimens’ quality, isolation of specific pathogens, alert reports for infection control practitioners, and real-time collection of lab trend data, all essential for the prevention and control of infections and epidemiological studies.
Conclusion
In conclusion, timely, accurate, and clinically relevant information is the basis for prevention and treatment of infections. Laboratory automation and laboratory informatics can greatly improve the accuracy of diagnostic procedures, TTR, and laboratory workflow. However, to exploit these technologies for the benefit of the patients, clinical microbiologists need to change their way of working—according to a lean workflow and a patient-centered approach—and their way of thinking, working more closely with clinical staff.
Abbreviations, acronyms, and initialisms
- AI: artificial intelligence
- AR: antimicrobial resistance
- AS: antimicrobial stewardship
- AST: antimicrobial susceptibility testing
- BC: blood culture
- ID: identification
- IT: information technology
- LIS: laboratory information system
- MALDI-TOF/MS: matrix-assisted laser desorption/ionization time-of-flight mass spectrometry
- MDR: multi-drug-resistant
- MDRO: multi-drug-resistant organism
- MRSA: methicillin-resistant Staphylococcus aureus
- NGS: next-generation sequencing
- QC: quality control
- QMS: quality management system
- TAT: turnaround time
- TLA: total laboratory automation
- TTR: time to report
- VRE: vancomycin-resistant enterococci
Acknowledgements
Author contributions
Study concept: AM, GD, EC. Critical revision of manuscript: PB, EP. Approval of manuscript: AM, GD, EC, PB, EP. All authors contributed to the article and approved the submitted version.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material. Further inquiries can be directed to the corresponding author.
Conflict of interest
AM has received funds for speaking at a symposium organized on behalf of Becton‐Dickinson. The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
- ↑ O'Neill, J. (May 2016). "Tackling drug-resistant infections globally: Final report and recommendations" (PDF). Review on Antimicrobial Resistance. pp. 80. https://amr-review.org/sites/default/files/160525_Final%20paper_with%20cover.pdf.
- ↑ Levy, Mitchell M.; Evans, Laura E.; Rhodes, Andrew (1 June 2018). "The Surviving Sepsis Campaign Bundle: 2018 update" (in en). Intensive Care Medicine 44 (6): 925–928. doi:10.1007/s00134-018-5085-0. ISSN 0342-4642. http://link.springer.com/10.1007/s00134-018-5085-0.
- ↑ Kumar, Anand; Ellis, Paul; Arabi, Yaseen; Roberts, Dan; Light, Bruce; Parrillo, Joseph E.; Dodek, Peter; Wood, Gordon et al. (1 November 2009). "Initiation of Inappropriate Antimicrobial Therapy Results in a Fivefold Reduction of Survival in Human Septic Shock" (in en). Chest 136 (5): 1237–1248. doi:10.1378/chest.09-0087. https://linkinghub.elsevier.com/retrieve/pii/S0012369209606796.
- ↑ Zilberberg, Marya D.; Nathanson, Brian H.; Sulham, Kate; Fan, Weihong; Shorr, Andrew F. (1 December 2017). "Carbapenem resistance, inappropriate empiric treatment and outcomes among patients hospitalized with Enterobacteriaceae urinary tract infection, pneumonia and sepsis" (in en). BMC Infectious Diseases 17 (1): 279. doi:10.1186/s12879-017-2383-z. ISSN 1471-2334. PMC PMC5393012. PMID 28415969. http://bmcinfectdis.biomedcentral.com/articles/10.1186/s12879-017-2383-z.
- ↑ Raman, Gowri; Avendano, Esther; Berger, Samantha; Menon, Vandana (1 December 2015). "Appropriate initial antibiotic therapy in hospitalized patients with gram-negative infections: systematic review and meta-analysis" (in en). BMC Infectious Diseases 15 (1): 395. doi:10.1186/s12879-015-1123-5. ISSN 1471-2334. PMC PMC4589179. PMID 26423743. http://bmcinfectdis.biomedcentral.com/articles/10.1186/s12879-015-1123-5.
- ↑ 6.0 6.1 6.2 Trotter, Alexander J.; Aydin, Alp; Strinden, Michael J.; O’Grady, Justin (1 October 2019). "Recent and emerging technologies for the rapid diagnosis of infection and antimicrobial resistance" (in en). Current Opinion in Microbiology 51: 39–45. doi:10.1016/j.mib.2019.03.001. https://linkinghub.elsevier.com/retrieve/pii/S1369527418301279.
- ↑ Messacar, Kevin; Parker, Sarah K.; Todd, James K.; Dominguez, Samuel R. (1 March 2017). Kraft, Colleen Suzanne. ed. "Implementation of Rapid Molecular Infectious Disease Diagnostics: the Role of Diagnostic and Antimicrobial Stewardship" (in en). Journal of Clinical Microbiology 55 (3): 715–723. doi:10.1128/JCM.02264-16. ISSN 0095-1137. PMC PMC5328439. PMID 28031432. https://journals.asm.org/doi/10.1128/JCM.02264-16.
- ↑ 8.0 8.1 Croxatto, A.; Prod'hom, G.; Faverjon, F.; Rochais, Y.; Greub, G. (1 March 2016). "Laboratory automation in clinical bacteriology: what system to choose?" (in en). Clinical Microbiology and Infection 22 (3): 217–235. doi:10.1016/j.cmi.2015.09.030. https://linkinghub.elsevier.com/retrieve/pii/S1198743X16000069.
- ↑ 9.0 9.1 Croxatto, Antony; Dijkstra, Klaas; Prod'hom, Guy; Greub, Gilbert (1 July 2015). Burnham, C. -A. D.. ed. "Comparison of Inoculation with the InoqulA and WASP Automated Systems with Manual Inoculation" (in en). Journal of Clinical Microbiology 53 (7): 2298–2307. doi:10.1128/JCM.03076-14. ISSN 0095-1137. PMC PMC4473203. PMID 25972424. https://journals.asm.org/doi/10.1128/JCM.03076-14.
- ↑ 10.0 10.1 Burckhardt, Irene (22 November 2018). "Laboratory Automation in Clinical Microbiology" (in en). Bioengineering 5 (4): 102. doi:10.3390/bioengineering5040102. ISSN 2306-5354. PMC PMC6315553. PMID 30467275. http://www.mdpi.com/2306-5354/5/4/102.
- ↑ Quiblier, Chantal; Jetter, Marion; Rominski, Mark; Mouttet, Forouhar; Böttger, Erik C.; Keller, Peter M.; Hombach, Michael (1 March 2016). Onderdonk, A. B.. ed. "Performance of Copan WASP for Routine Urine Microbiology" (in en). Journal of Clinical Microbiology 54 (3): 585–592. doi:10.1128/JCM.02577-15. ISSN 0095-1137. PMC PMC4767997. PMID 26677255. https://journals.asm.org/doi/10.1128/JCM.02577-15.
- ↑ Iversen, Jesper; Stendal, Gitta; Gerdes, Cecilie M.; Meyer, Christian H.; Andersen, Christian Østergaard; Frimodt-Møller, Niels (1 February 2016). Ledeboer, N. A.. ed. "Comparative Evaluation of Inoculation of Urine Samples with the Copan WASP and BD Kiestra InoqulA Instruments" (in en). Journal of Clinical Microbiology 54 (2): 328–332. doi:10.1128/JCM.01718-15. ISSN 0095-1137. PMC PMC4733172. PMID 26607980. https://journals.asm.org/doi/10.1128/JCM.01718-15.
- ↑ 13.0 13.1 13.2 Croxatto, Antony; Marcelpoil, Raphaël; Orny, Cédrick; Morel, Didier; Prod'hom, Guy; Greub, Gilbert (1 December 2017). "Towards automated detection, semi-quantification and identification of microbial growth in clinical bacteriology: A proof of concept" (in en). Biomedical Journal 40 (6): 317–328. doi:10.1016/j.bj.2017.09.001. PMC PMC6138813. PMID 29433835. https://linkinghub.elsevier.com/retrieve/pii/S2319417017302834.
- ↑ Cheng, C.W.R.; Ong, C.H.; Chan, D.S.G. (1 September 2020). "Impact of BD Kiestra InoqulA streaking patterns on colony isolation and turnaround time of methicillin-resistant Staphylococcus aureus and carbapenem-resistant Enterobacterale surveillance samples" (in en). Clinical Microbiology and Infection 26 (9): 1201–1206. doi:10.1016/j.cmi.2020.01.006. https://linkinghub.elsevier.com/retrieve/pii/S1198743X20300288.
- ↑ 15.0 15.1 Burckhardt, Irene; Last, Katharina; Zimmermann, Stefan (28 January 2019). "Shorter Incubation Times for Detecting Multi-drug Resistant Bacteria in Patient Samples: Defining Early Imaging Time Points Using Growth Kinetics and Total Laboratory Automation" (in en). Annals of Laboratory Medicine 39 (1): 43–49. doi:10.3343/alm.2019.39.1.43. ISSN 2234-3806. PMC PMC6143461. PMID 30215229. http://annlabmed.org/journal/view.html?doi=10.3343/alm.2019.39.1.43.
- ↑ Moreno-Camacho, José L; Calva-Espinosa, Diana Y; Leal-Leyva, Yoseli Y; Elizalde-Olivas, Dolores C; Campos-Romero, Abraham; Alcántar-Fernández, Jonathan (1 January 2018). "Transformation From a Conventional Clinical Microbiology Laboratory to Full Automation" (in en). Laboratory Medicine 49 (1): e1–e8. doi:10.1093/labmed/lmx079. ISSN 0007-5027. https://academic.oup.com/labmed/article/49/1/e1/4743273.
- ↑ 17.0 17.1 Theparee, Talent; Das, Sanchita; Thomson, Richard B. (1 January 2018). Patel, Robin. ed. "Total Laboratory Automation and Matrix-Assisted Laser Desorption Ionization–Time of Flight Mass Spectrometry Improve Turnaround Times in the Clinical Microbiology Laboratory: a Retrospective Analysis" (in en). Journal of Clinical Microbiology 56 (1): e01242–17. doi:10.1128/JCM.01242-17. ISSN 0095-1137. PMC PMC5744220. PMID 29118171. https://journals.asm.org/doi/10.1128/JCM.01242-17.
- ↑ Cherkaoui, A.; Renzi, G.; Vuilleumier, N.; Schrenzel, J. (1 November 2019). "Copan WASPLab automation significantly reduces incubation times and allows earlier culture readings" (in en). Clinical Microbiology and Infection 25 (11): 1430.e5–1430.e12. doi:10.1016/j.cmi.2019.04.001. https://linkinghub.elsevier.com/retrieve/pii/S1198743X19301521.
- ↑ Thomson, Richard B.; McElvania, Erin (1 September 2019). "Total Laboratory Automation" (in en). Clinics in Laboratory Medicine 39 (3): 371–389. doi:10.1016/j.cll.2019.05.002. https://linkinghub.elsevier.com/retrieve/pii/S0272271219300290.
- ↑ 20.0 20.1 Cherkaoui, Abdessalam; Schrenzel, Jacques (3 February 2022). "Total Laboratory Automation for Rapid Detection and Identification of Microorganisms and Their Antimicrobial Resistance Profiles". Frontiers in Cellular and Infection Microbiology 12: 807668. doi:10.3389/fcimb.2022.807668. ISSN 2235-2988. PMC PMC8851030. PMID 35186794. https://www.frontiersin.org/articles/10.3389/fcimb.2022.807668/full.
- ↑ Cherkaoui, Abdessalam; Riat, Arnaud; Renzi, Gesuele; Fischer, Adrien; Schrenzel, Jacques (1 February 2023). "Diagnostic test accuracy of an automated device for the MALDI target preparation for microbial identification" (in en). European Journal of Clinical Microbiology & Infectious Diseases 42 (2): 153–159. doi:10.1007/s10096-022-04531-3. ISSN 0934-9723. PMC PMC9836989. PMID 36469165. https://link.springer.com/10.1007/s10096-022-04531-3.
- ↑ 22.0 22.1 22.2 Jacot, Damien; Sarton-Lohéac, Garance; Coste, Alix T.; Bertelli, Claire; Greub, Gilbert; Prod'hom, Guy; Croxatto, Antony (1 August 2021). "Performance evaluation of the Becton Dickinson Kiestra™ IdentifA/SusceptA" (in en). Clinical Microbiology and Infection 27 (8): 1167.e9–1167.e17. doi:10.1016/j.cmi.2020.09.050. https://linkinghub.elsevier.com/retrieve/pii/S1198743X20306042.
- ↑ Cherkaoui, Abdessalam; Renzi, Gesuele; Vuilleumier, Nicolas; Schrenzel, Jacques (18 August 2021). McElvania, Erin. ed. "Performance of Fully Automated Antimicrobial Disk Diffusion Susceptibility Testing Using Copan WASP Colibri Coupled to the Radian In-Line Carousel and Expert System" (in en). Journal of Clinical Microbiology 59 (9): e00777–21. doi:10.1128/JCM.00777-21. ISSN 0095-1137. PMC PMC8373016. PMID 34160274. https://journals.asm.org/doi/10.1128/JCM.00777-21.
- ↑ 24.0 24.1 Faron, Matthew L.; Buchan, Blake W.; Vismara, Chiara; Lacchini, Carla; Bielli, Alessandra; Gesu, Giovanni; Liebregts, Theo; van Bree, Anita et al. (1 March 2016). Richter, S. S.. ed. "Automated Scoring of Chromogenic Media for Detection of Methicillin-Resistant Staphylococcus aureus by Use of WASPLab Image Analysis Software" (in en). Journal of Clinical Microbiology 54 (3): 620–624. doi:10.1128/JCM.02778-15. ISSN 0095-1137. PMC PMC4767952. PMID 26719443. https://journals.asm.org/doi/10.1128/JCM.02778-15.
- ↑ 25.0 25.1 Faron, Matthew L.; Buchan, Blake W.; Coon, Christopher; Liebregts, Theo; van Bree, Anita; Jansz, Arjan R.; Soucy, Genevieve; Korver, John et al. (1 October 2016). Burnham, C.-A. D.. ed. "Automatic Digital Analysis of Chromogenic Media for Vancomycin-Resistant-Enterococcus Screens Using Copan WASPLab" (in en). Journal of Clinical Microbiology 54 (10): 2464–2469. doi:10.1128/JCM.01040-16. ISSN 0095-1137. PMC PMC5035414. PMID 27413193. https://journals.asm.org/doi/10.1128/JCM.01040-16.
- ↑ Foschi, Claudio; Gaibani, Paolo; Lombardo, Donatella; Re, Maria Carla; Ambretti, Simone (1 June 2020). "Rectal screening for carbapenemase-producing Enterobacteriaceae: a proposed workflow" (in en). Journal of Global Antimicrobial Resistance 21: 86–90. doi:10.1016/j.jgar.2019.10.012. https://linkinghub.elsevier.com/retrieve/pii/S2213716519302668.
- ↑ Dauwalder, O.; Landrieve, L.; Laurent, F.; de Montclos, M.; Vandenesch, F.; Lina, G. (1 March 2016). "Does bacteriology laboratory automation reduce time to results and increase quality management?" (in en). Clinical Microbiology and Infection 22 (3): 236–243. doi:10.1016/j.cmi.2015.10.037. https://linkinghub.elsevier.com/retrieve/pii/S1198743X15009787.
- ↑ Tabak, Ying P.; Vankeepuram, Latha; Ye, Gang; Jeffers, Kay; Gupta, Vikas; Murray, Patrick R. (1 December 2018). Carroll, Karen C.. ed. "Blood Culture Turnaround Time in U.S. Acute Care Hospitals and Implications for Laboratory Process Optimization" (in en). Journal of Clinical Microbiology 56 (12): e00500–18. doi:10.1128/JCM.00500-18. ISSN 0095-1137. PMC PMC6258864. PMID 30135230. https://journals.asm.org/doi/10.1128/JCM.00500-18.
- ↑ 29.0 29.1 De Socio, Giuseppe Vittorio; Di Donato, Francesco; Paggi, Riccardo; Gabrielli, Chiara; Belati, Alessandra; Rizza, Giuseppe; Savoia, Martina; Repetto, Antonella et al. (1 December 2018). "Laboratory automation reduces time to report of positive blood cultures and improves management of patients with bloodstream infection" (in en). European Journal of Clinical Microbiology & Infectious Diseases 37 (12): 2313–2322. doi:10.1007/s10096-018-3377-5. ISSN 0934-9723. http://link.springer.com/10.1007/s10096-018-3377-5.
- ↑ Vandenberg, Olivier; Durand, Géraldine; Hallin, Marie; Diefenbach, Andreas; Gant, Vanya; Murray, Patrick; Kozlakidis, Zisis; van Belkum, Alex (18 March 2020). "Consolidation of Clinical Microbiology Laboratories and Introduction of Transformative Technologies" (in en). Clinical Microbiology Reviews 33 (2): e00057–19. doi:10.1128/CMR.00057-19. ISSN 0893-8512. PMC PMC7048017. PMID 32102900. https://journals.asm.org/doi/10.1128/CMR.00057-19.
- ↑ Kulengowski, B.; Ribes, J.A.; Burgess, D.S. (1 January 2019). "Polymyxin B Etest® compared with gold-standard broth microdilution in carbapenem-resistant Enterobacteriaceae exhibiting a wide range of polymyxin B MICs" (in en). Clinical Microbiology and Infection 25 (1): 92–95. doi:10.1016/j.cmi.2018.04.008. https://linkinghub.elsevier.com/retrieve/pii/S1198743X18303434.
- ↑ Camarlinghi, Giulio; Parisio, Eva Maria; Antonelli, Alberto; Nardone, Maria; Coppi, Marco; Giani, Tommaso; Mattei, Romano; Rossolini, Gian Maria (1 January 2019). "Discrepancies in fosfomycin susceptibility testing of KPC-producing Klebsiella pneumoniae with various commercial methods" (in en). Diagnostic Microbiology and Infectious Disease 93 (1): 74–76. doi:10.1016/j.diagmicrobio.2018.07.014. https://linkinghub.elsevier.com/retrieve/pii/S0732889318302505.
- ↑ Simner, Patricia J.; Patel, Robin (17 December 2020). Burnham, Carey-Ann D.. ed. "Cefiderocol Antimicrobial Susceptibility Testing Considerations: the Achilles' Heel of the Trojan Horse?" (in en). Journal of Clinical Microbiology 59 (1): e00951–20. doi:10.1128/JCM.00951-20. ISSN 0095-1137. PMC PMC7771437. PMID 32727829. https://journals.asm.org/doi/10.1128/JCM.00951-20.
- ↑ Antonelli, Alberto; Giani, Tommaso; Di Pilato, Vincenzo; Riccobono, Eleonora; Perriello, Gabriele; Mencacci, Antonella; Rossolini, Gian Maria (1 August 2019). "KPC-31 expressed in a ceftazidime/avibactam-resistant Klebsiella pneumoniae is associated with relevant detection issues" (in en). Journal of Antimicrobial Chemotherapy 74 (8): 2464–2466. doi:10.1093/jac/dkz156. ISSN 0305-7453. https://academic.oup.com/jac/article/74/8/2464/5477394.
- ↑ 35.0 35.1 De Socio, Giuseppe Vittorio; Rubbioni, Paola; Botta, Daniele; Cenci, Elio; Belati, Alessandra; Paggi, Riccardo; Pasticci, Maria Bruna; Mencacci, Antonella (1 December 2019). "Measurement and prediction of antimicrobial resistance in bloodstream infections by ESKAPE pathogens and Escherichia coli" (in en). Journal of Global Antimicrobial Resistance 19: 154–160. doi:10.1016/j.jgar.2019.05.013. https://linkinghub.elsevier.com/retrieve/pii/S2213716519301237.
- ↑ Culbreath, Karissa; Piwonka, Heather; Korver, John; Noorbakhsh, Mir (18 February 2021). McElvania, Erin. ed. "Benefits Derived from Full Laboratory Automation in Microbiology: a Tale of Four Laboratories" (in en). Journal of Clinical Microbiology 59 (3): e01969–20. doi:10.1128/JCM.01969-20. ISSN 0095-1137. PMC PMC8106725. PMID 33239383. https://journals.asm.org/doi/10.1128/JCM.01969-20.
- ↑ 37.0 37.1 Zimmermann, Stefan (18 February 2021). McElvania, Erin. ed. "Laboratory Automation in the Microbiology Laboratory: an Ongoing Journey, Not a Tale?" (in en). Journal of Clinical Microbiology 59 (3): e02592–20. doi:10.1128/JCM.02592-20. ISSN 0095-1137. PMC PMC8106703. PMID 33361341. https://journals.asm.org/doi/10.1128/JCM.02592-20.
- ↑ Womack, James P.; Jones, Daniel T.; Roos, Daniel (1990). The machine that changed the world: the story of lean production - Toyota´s secret weapon in the global car wars that is revolutionizing world industry (1. paperback ed ed.). London: Free Press. ISBN 978-0-7432-9979-4.
- ↑ Yarbrough, Melanie L.; Lainhart, William; McMullen, Allison R.; Anderson, Neil W.; Burnham, Carey-Ann D. (1 December 2018). "Impact of total laboratory automation on workflow and specimen processing time for culture of urine specimens" (in en). European Journal of Clinical Microbiology & Infectious Diseases 37 (12): 2405–2411. doi:10.1007/s10096-018-3391-7. ISSN 0934-9723. http://link.springer.com/10.1007/s10096-018-3391-7.
- ↑ Burckhardt, Irene; Horner, Susanne; Burckhardt, Florian; Zimmermann, Stefan (1 September 2018). "Detection of MRSA in nasal swabs—marked reduction of time to report for negative reports by substituting classical manual workflow with total lab automation" (in en). European Journal of Clinical Microbiology & Infectious Diseases 37 (9): 1745–1751. doi:10.1007/s10096-018-3308-5. ISSN 0934-9723. PMC PMC6133036. PMID 29943308. http://link.springer.com/10.1007/s10096-018-3308-5.
- ↑ Seng, Piseth; Drancourt, Michel; Gouriet, Frédérique; La Scola, Bernard; Fournier, Pierre‐Edouard; Rolain, Jean Marc; Raoult, Didier (15 August 2009). "Ongoing Revolution in Bacteriology: Routine Identification of Bacteria by Matrix‐Assisted Laser Desorption Ionization Time‐of‐Flight Mass Spectrometry" (in en). Clinical Infectious Diseases 49 (4): 543–551. doi:10.1086/600885. ISSN 1058-4838. https://academic.oup.com/cid/article-lookup/doi/10.1086/600885.
- ↑ Charnot-Katsikas, Angella; Tesic, Vera; Love, Nedra; Hill, Brandy; Bethel, Cindy; Boonlayangoor, Sue; Beavis, Kathleen G. (1 January 2018). Bourbeau, Paul. ed. "Use of the Accelerate Pheno System for Identification and Antimicrobial Susceptibility Testing of Pathogens in Positive Blood Cultures and Impact on Time to Results and Workflow" (in en). Journal of Clinical Microbiology 56 (1): e01166–17. doi:10.1128/JCM.01166-17. ISSN 0095-1137. PMC PMC5744213. PMID 29118168. https://journals.asm.org/doi/10.1128/JCM.01166-17.
- ↑ 43.0 43.1 Arena, Fabio; Giani, Tommaso; Pollini, Simona; Viaggi, Bruno; Pecile, Patrizia; Rossolini, Gian Maria (1 April 2017). "Molecular antibiogram in diagnostic clinical microbiology: advantages and challenges" (in en). Future Microbiology 12 (5): 361–364. doi:10.2217/fmb-2017-0019. ISSN 1746-0913. https://www.futuremedicine.com/doi/10.2217/fmb-2017-0019.
- ↑ Mitchell, Stephanie L.; Simner, Patricia J. (1 September 2019). "Next-Generation Sequencing in Clinical Microbiology" (in en). Clinics in Laboratory Medicine 39 (3): 405–418. doi:10.1016/j.cll.2019.05.003. https://linkinghub.elsevier.com/retrieve/pii/S0272271219300307.
- ↑ Pitashny, Milena; Kadry, Balqees; Shalaginov, Raya; Gazit, Liat; Zohar, Yaniv; Szwarcwort, Moran; Stabholz, Yoav; Paul, Mical (19 October 2022). "NGS in the clinical microbiology settings". Frontiers in Cellular and Infection Microbiology 12: 955481. doi:10.3389/fcimb.2022.955481. ISSN 2235-2988. PMC PMC9627026. PMID 36339334. https://www.frontiersin.org/articles/10.3389/fcimb.2022.955481/full.
- ↑ Anandan, Shalini (2015). "Rapid Screening for Carbapenem Resistant Organisms: Current Results and Future Approaches". JOURNAL OF CLINICAL AND DIAGNOSTIC RESEARCH. doi:10.7860/JCDR/2015/14246.6530. PMC PMC4606238. PMID 26500909. http://jcdr.net/article_fulltext.asp?issn=0973-709x&year=2015&volume=9&issue=9&page=DM01&issn=0973-709x&id=6530.
- ↑ 47.0 47.1 Ambretti, Simone; Bassetti, Matteo; Clerici, Pierangelo; Petrosillo, Nicola; Tumietto, Fabio; Viale, Pierluigi; Rossolini, Gian Maria (1 December 2019). "Screening for carriage of carbapenem-resistant Enterobacteriaceae in settings of high endemicity: a position paper from an Italian working group on CRE infections" (in en). Antimicrobial Resistance & Infection Control 8 (1): 136. doi:10.1186/s13756-019-0591-6. ISSN 2047-2994. PMC PMC6693230. PMID 31423299. https://aricjournal.biomedcentral.com/articles/10.1186/s13756-019-0591-6.
- ↑ Mangioni, Davide; Viaggi, Bruno; Giani, Tommaso; Arena, Fabio; D'Arienzo, Sara; Forni, Silvia; Tulli, Giorgio; Rossolini, Gian M (1 February 2019). "Diagnostic stewardship for sepsis: the need for risk stratification to triage patients for fast microbiology workflows" (in en). Future Microbiology 14 (3): 169–174. doi:10.2217/fmb-2018-0329. ISSN 1746-0913. https://www.futuremedicine.com/doi/10.2217/fmb-2018-0329.
- ↑ Skodvin, Brita; Aase, Karina; Brekken, Anita Løvås; Charani, Esmita; Lindemann, Paul Christoffer; Smith, Ingrid (1 September 2017). "Addressing the key communication barriers between microbiology laboratories and clinical units: a qualitative study" (in en). Journal of Antimicrobial Chemotherapy 72 (9): 2666–2672. doi:10.1093/jac/dkx163. ISSN 0305-7453. PMC PMC5890706. PMID 28633405. https://academic.oup.com/jac/article/72/9/2666/3867670.
- ↑ Tiseo, Giusy; Brigante, Gioconda; Giacobbe, Daniele Roberto; Maraolo, Alberto Enrico; Gona, Floriana; Falcone, Marco; Giannella, Maddalena; Grossi, Paolo et al. (1 August 2022). "Diagnosis and management of infections caused by multidrug-resistant bacteria: guideline endorsed by the Italian Society of Infection and Tropical Diseases (SIMIT), the Italian Society of Anti-Infective Therapy (SITA), the Italian Group for Antimicrobial Stewardship (GISA), the Italian Association of Clinical Microbiologists (AMCLI) and the Italian Society of Microbiology (SIM)" (in en). International Journal of Antimicrobial Agents 60 (2): 106611. doi:10.1016/j.ijantimicag.2022.106611. https://linkinghub.elsevier.com/retrieve/pii/S0924857922001236.
Notes
This presentation is faithful to the original, with only a few minor changes to presentation. In some cases important information was missing from the references, and that information was added. The original article lists references alphabetically; they are listed by order of appearance for this version, by design.