Difference between revisions of "Journal:Best practice recommendations for the implementation of a digital pathology workflow in the anatomic pathology laboratory by the European Society of Digital and Integrative Pathology (ESDIP)"
Shawndouglas (talk | contribs) (Saving and adding more.) |
Shawndouglas (talk | contribs) (Saving and adding more.) |
||
| Line 169: | Line 169: | ||
===Embedding checkpoints=== | ===Embedding checkpoints=== | ||
Once the processed specimen inside the cassettes have arrived at the embedding room, operators (technicians) should be able to access the pictures taken during the grossing phase by simply scanning the barcode (Table 2). This will allow them to compare them with the content of cassettes after processing, checking their correspondence to rule out the loss of biological material. Correct embedding may prevent the creation of poor-quality virtual slides. One of the possible issues during the scanning phase is represented by the presence of large fragments, which are more prone to be hydrated during the processing steps and thus more complicated to be captured by the scanner. To address this problem, the fragments should be reduced during the grossing phase, and the embedding checkpoint is essential to control this point. Similarly, tissue fragments well oriented, levelled, and close to each other in paraffin, may constitute good substrates for better-quality glass slides. If the sample to be analyzed is too large to be fitted in a regular glass slide, the recent introduction of dedicated scanners for “macro” glass slides provides the possibility of this solution directly from the grossing room.<ref>{{Cite journal |last=Pantanowitz |first=Liron |last2=Farahani |first2=Navid |last3=Parwani |first3=Anil |date=2015-06 |title=Whole slide imaging in pathology: advantages, limitations, and emerging perspectives |url=http://www.dovepress.com/whole-slide-imaging-in-pathology-advantages-limitations-and-emerging-p-peer-reviewed-article-PLMI |journal=Pathology and Laboratory Medicine International |language=en |pages=23–33 |doi=10.2147/PLMI.S59826 |issn=1179-2698}}</ref> | Once the processed specimen inside the cassettes have arrived at the embedding room, operators (technicians) should be able to access the pictures taken during the grossing phase by simply scanning the barcode (Table 2). This will allow them to compare them with the content of cassettes after processing, checking their correspondence to rule out the loss of biological material. Correct embedding may prevent the creation of poor-quality virtual slides. One of the possible issues during the scanning phase is represented by the presence of large fragments, which are more prone to be hydrated during the processing steps and thus more complicated to be captured by the scanner. To address this problem, the fragments should be reduced during the grossing phase, and the embedding checkpoint is essential to control this point. Similarly, tissue fragments well oriented, levelled, and close to each other in paraffin, may constitute good substrates for better-quality glass slides. If the extracted sample to be analyzed is too large to be fitted in a regular glass slide, the recent introduction of dedicated scanners for “macro” glass slides provides the possibility of this solution directly from the grossing room.<ref>{{Cite journal |last=Pantanowitz |first=Liron |last2=Farahani |first2=Navid |last3=Parwani |first3=Anil |date=2015-06 |title=Whole slide imaging in pathology: advantages, limitations, and emerging perspectives |url=http://www.dovepress.com/whole-slide-imaging-in-pathology-advantages-limitations-and-emerging-p-peer-reviewed-article-PLMI |journal=Pathology and Laboratory Medicine International |language=en |pages=23–33 |doi=10.2147/PLMI.S59826 |issn=1179-2698}}</ref> | ||
===Sectioning checkpoints=== | ===Sectioning checkpoints=== | ||
| Line 193: | Line 193: | ||
|- | |- | ||
|} | |} | ||
===Staining and mounting checkpoints=== | |||
Once in the staining workstation, the slides produced in the digital workflow are identified through their code to define which staining protocol they should follow, as per internal LIS prerecorded indications, using automated staining platforms. As in the previous step, the staining process should follow the highest qualitative standards to reduce possible modifications that can interfere with the scanning phase (faint or darker staining, debris/precipitates). For this purpose, implementing an internal checkpoint with daily controls and/or external quality control can help assess the quality of stained slides.<ref>{{Cite journal |last=Janowczyk |first=Andrew |last2=Zuo |first2=Ren |last3=Gilmore |first3=Hannah |last4=Feldman |first4=Michael |last5=Madabhushi |first5=Anant |date=2019-12 |title=HistoQC: An Open-Source Quality Control Tool for Digital Pathology Slides |url=https://ascopubs.org/doi/10.1200/CCI.18.00157 |journal=JCO Clinical Cancer Informatics |language=en |volume=3 |issue= |pages=1–7 |doi=10.1200/CCI.18.00157 |issn=2473-4276 |pmc=PMC6552675 |pmid=30990737}}</ref> Automating the staining may contribute to a stable result, allowing the design of a scanning protocol applicable to most of the slides, avoiding restaining and rescanning slides. The production of consistent staining with a clean background is relevant because it decreases the size of the produced digital slides. A final word is needed to address the mounting process and respective automation. To minimize the interference of the mounting medium in the scanning process, the laboratory must select the mounter, the coverslip type, and respective mounting medium to be used in all sorts of glass slides so that the scanner can be calibrated accordingly. Before the scanning phase, it is of paramount importance to check whether the slide is in an adequate state for scanning. After the staining/cover-slipping phase, it should be dry to prevent scanning problems (e.g., stitching, blurring, out of focus areas). Moreover, the scanning phase can be either affected by the different positions of the coverslips, leading to a misalignment of the slides in the rack. Differences in the type of coverslip can be responsible for a high rate of WSIs being out of focus. The use of automatic mounters obviates variations in the quality of the mounting and prevents errors if an adequate revision of the mounter is provided. | |||
===Correcting assigning of the WSI to the case checkpoints=== | |||
This topic is discussed further in the next section on scanning. | |||
===Archiving checkpoints=== | |||
After the sectioning and scanning phases, blocks and slides can be appropriately archived to be retrieved whenever is necessary. This task has been historically performed manually by operators (technicians or laboratory assistants), leading to loss and misplacement of blocks/slides, with obvious medico-legal consequences. Moreover, the wide practice of consulting archival material by all the laboratory workers, including residents and students for didactic purposes, can further complicate the correct positioning of these specimens. Based on these observations, full integration with the LIS and the presence of unique identifiers, both on the blocks and glass slides, allow for a more procedural yet automated archiving of all the biological material, as well as its safe and unbiased retrieval if needed when, for example, a request of external consultation arrives. (For archiving of the WSI, please refer to the data retention policy, discussed later in the section on "Validation of WSI for clinical use.") | |||
==Scanner for slide digitization== | |||
This section contains some considerations and recommendations for selecting and managing the most appropriate digital slide scanner, given a set or requirements for the scanning phase (Table 4). As in other medical specialties, which have been dramatically changed by the introduction of a wide variety of digital devices for routine daily work<ref>{{Cite journal |last=Ferrini |first=Francesco |last2=Sannino |first2=Gianpaolo |last3=Chiola |first3=Carlo |last4=Capparé |first4=Paolo |last5=Gastaldi |first5=Giorgio |last6=Gherlone |first6=Enrico |date=2019-02-14 |title=Influence of Intra-Oral Scanner (I.O.S.) on The Marginal Accuracy of CAD/CAM Single Crowns |url=http://www.mdpi.com/1660-4601/16/4/544 |journal=International Journal of Environmental Research and Public Health |language=en |volume=16 |issue=4 |pages=544 |doi=10.3390/ijerph16040544 |issn=1660-4601 |pmc=PMC6406818 |pmid=30769768}}</ref>, it is not the focus of the present recommendations to draw a meticulous review of the technical characteristics of a scanner, since several studies have already been published on this subject.<ref>{{Cite journal |last=Hufnagl |first=Peter |last2=Zwönitzer |first2=Ralf |last3=Haroske |first3=Gunter |date=2018-09-08 |title=Guidelines Digital Pathology for Diagnosis on (and Reports of) Digital Images Version 1.0 Bundesverband deutscher Pathologen e.V. (Federal Association of German Pathologist) |url=http://www.diagnosticpathology.eu/content/index.php/dpath/article/view/266 |journal=Diagnostic Pathology |language=en |volume=4 |issue=1 |pages=266 |at= |doi=10.17629/WWW.DIAGNOSTICPATHOLOGY.EU-2018-4:266}}</ref><ref>{{Cite web |last=Cross, S.; Furness, P.; Igali, L. et al. |date=January 2018 |title=Best practice recommendations for implementing digital pathology |url=https://www.rcpath.org/uploads/assets/f465d1b3-797b-4297-b7fedc00b4d77e51/Best-practice-recommendations-for-implementing-digital-pathology.pdf |format=PDF |publisher=The Royal College of Pathologists |accessdate=10 November 2021}}</ref> | |||
{| class="wikitable" border="1" cellpadding="5" cellspacing="0" width="60%" | |||
|- | |||
| colspan="1" style="background-color:white; padding-left:10px; padding-right:10px;" |'''Table 4.''' Recommendations for the scanning phase | |||
|- | |||
! style="background-color:#dddddd; padding-left:10px; padding-right:10px;" |Scanning checkpoints | |||
|- | |||
| style="background-color:white; padding-left:10px; padding-right:10px;" |1. At any given time, two scanners digitize twice the number of slides compared to a single scanner, and three scanners triple this (e.g., for a caseload of 300 slides per day, employing three scanners with 100-slide capacity could be better than using a single scanner with a 300-slide capacity). | |||
|- | |||
| style="background-color:white; padding-left:10px; padding-right:10px;" |2. It is advisable to scan during the daytime, with the lab personnel present to solve unexpected problems. | |||
|- | |||
| style="background-color:white; padding-left:10px; padding-right:10px;" |3. Scanning sessions during the night might be problematic in some already established workflows; thus, if there are problems with the scanning process, it might be better to avoid scanning after working hours. | |||
|- | |||
| style="background-color:white; padding-left:10px; padding-right:10px;" |4. A single-scanner approach is not recommended when contemplating a daily routine diagnostic workflow. | |||
|- | |||
| style="background-color:white; padding-left:10px; padding-right:10px;" |5. Consider the possibility of a continuous loading and eventual prioritization of a batch of slides. | |||
|- | |||
|} | |||
The most appropriate scanner should be selected based on the needs of the specific laboratory (e.g., primary diagnosis, consultation, education, and research). The following section focuses on the possible impact of such a choice on DP workflow implementation. According to the LEAN approach, as discussed earlier, the positioning of the scanners should follow the logic of an automated workflow and thus be placed as close as possible to the staining and cover-slipping stations, making their implementation in the entire process easier and smoother.<ref name=":0" /><ref name=":1" /> | |||
The transition to digital pathology also includes choosing the most appropriate types and numbers of scanners for the lab. Although it is highly dependent on the needs of each specific laboratory, one way to estimate the number of scanners is to review previous DP experiences.<ref name=":0" /><ref name=":1" /> In this context, each department should be aware of the expected application of the scanners, the total time required for the scanning process, and the time that can be dedicated to this part of the workflow. Some formulas to calculate the numbers of scanners needed in the lab have been proposed.<ref name=":0" /><ref name=":1" /> | |||
However, many variables must be considered when calculating the number of scanners required to digitize the entire slide volume within the same workday, thus not interfering with the turn-around time (TAT). These variables are limited by the technical specifications of the scanners and their related informatics networks (including bandwidth and switches) and the type and location of storage, together with the existing workflow within the lab (i.e., availability of personnel at all times of the day). One of the possible pitfalls in calculating the actual scanning time per slide/batch, and thus the number of scanners required per lab, could be represented by the reported scanning times by each vendor, generally calculated on a specimen tissue of 1.5 cm × 1.5 cm in size and with a local storage solution. However, this is far away from the routine practice of an anatomic pathology laboratory that must accommodate very small pieces of tissue (e.g., biopsies) as well as large surgical specimens, and that may even have the possibility of storing the WSI remotely or in the [[Cloud computing|cloud]]. Moreover, since the implementation of scanners should not impact the existing workflow and eventually lead to its improvement, there is a need to evaluate a continuous loading capability to preserve the same or similar workloads over time compared to the conventional analogue counterpart. This should be coupled with the possibility of prioritizing a specific batch of slides. | |||
A few additional comments are needed at this point. Broadly speaking, scanning during working hours should be preferred for practical and logistical reasons. If there are problems with the scanning process, it might be better to avoid scanning after working hours. For example, it has been reported that the mean scanning time in a routine environment is about six minutes for scanning a slide at an equivalent of 40 × magnification.<ref>{{Cite journal |last=Hanna |first=Matthew G. |last2=Reuter |first2=Victor E. |last3=Hameed |first3=Meera R. |last4=Tan |first4=Lee K. |last5=Chiang |first5=Sarah |last6=Sigel |first6=Carlie |last7=Hollmann |first7=Travis |last8=Giri |first8=Dilip |last9=Samboy |first9=Jennifer |last10=Moradel |first10=Carlos |last11=Rosado |first11=Andrea |date=2019-07 |title=Whole slide imaging equivalency and efficiency study: experience at a large academic center |url=http://www.nature.com/articles/s41379-019-0205-0 |journal=Modern Pathology |language=en |volume=32 |issue=7 |pages=916–928 |doi=10.1038/s41379-019-0205-0 |issn=0893-3952}}</ref> Therefore, it takes about four hours for one rack of 40 slides, and up to 40 hours to digitize all of the slides that fit inside the scanner (using an AT2, Leica Biosystems, Nussloch, Germany). However, it is well known that the scanning process may stop for several reasons, including sticky glass, connection problems, or software and hardware problems. The result may be an incomplete digitization of slides, with a consequent interruption of routine workflow in the subsequent morning. Based on the previous observations, and since the scanning process should be a continuous workflow in the lab, scanning during the day should be preferred to the overnight approach. This could enable lab personnel to react to the possible technical issues mentioned above. This could even lead to modifications in other parts of the pathology workflow to adapt routine specimen processing to the loading schedules required by the scanners. | |||
In this setting, the laboratory can choose to switch from bulk production of slides at the end of the day to a more continuous production of derived samples. Once the number of scanners needed and the required scanning time has been defined, the laboratory should verify whether the number of working operators employed in the department is sufficient to run the instruments for the specified length of time. Otherwise, the calculation of the necessary personnel is required, considering both 1. the scanning process and 2. any virtual slide quality control. The scanning process mainly consists of loading/unloading slides in the scanner and taking snapshots to ensure that the instrument captures all the material on the glass. On the other hand, the quality control phase is equally important and may be time-consuming, encompassing all the quality check procedures of the final WSI and related data. | |||
The points discussed above pertain to “regular” scanners for bright field microscopy. Other “special” scanners exist, e.g., those for dark field microscopy (immunofluorescence and fluorescence in-situ hybridization [FISH]), as well as those for whole mount slides (macro slides). Because of their highly specific fields of application<ref>{{Cite journal |last=L’Imperio |first=Vincenzo |last2=Brambilla |first2=Virginia |last3=Cazzaniga |first3=Giorgio |last4=Ferrario |first4=Franco |last5=Nebuloni |first5=Manuela |last6=Pagni |first6=Fabio |date=2021-06 |title=Digital pathology for the routine diagnosis of renal diseases: a standard model |url=https://link.springer.com/10.1007/s40620-020-00805-1 |journal=Journal of Nephrology |language=en |volume=34 |issue=3 |pages=681–688 |doi=10.1007/s40620-020-00805-1 |issn=1121-8428 |pmc=PMC8192318 |pmid=32683656}}</ref>, they are not the object of these recommendations. | |||
==Validation of WSI for clinical use== | |||
Revision as of 21:29, 5 December 2021
| Full article title | Best practice recommendations for the implementation of a digital pathology workflow in the anatomic pathology laboratory by the European Society of Digital and Integrative Pathology (ESDIP) |
|---|---|
| Journal | Diagnostics |
| Author(s) | Fraggetta, Filippo; L'Imperio, Vincenzo; Ameisen, David; Carvalho, Rita; Leh, Sabine; Kiehl, Tim-Rasmus; Serbanescu, Mircea; Racoceanu, Daniel; Mea, Vincenzo D.; Polonia, Antonio; Zerbe, Norman; Eloy, Catarina |
| Author affiliation(s) | European Society of Digital and Integrative Pathology, Azienda Sanitaria Provinciale Di Catania, University of Milano-Bicocca, Imginit SAS, Charité – Universitätsmedizin Berlin, Haukeland University Hospital, University of Bergen, University of Medicine and Pharmacy of Craiova, Sorbonne Université, University of Udine |
| Primary contact | Email: celoy at ipatimup dot pt |
| Year published | 2021 |
| Volume and issue | 11(11) |
| Article # | 2167 |
| DOI | 10.3390/diagnostics11112167 |
| ISSN | 2075-4418 |
| Distribution license | Creative Commons Attribution 4.0 International |
| Website | https://www.mdpi.com/2075-4418/11/11/2167/htm |
| Download | https://www.mdpi.com/2075-4418/11/11/2167/pdf (PDF) |
|
|
This article should be considered a work in progress and incomplete. Consider this article incomplete until this notice is removed. |
Abstract
The interest in implementing digital pathology (DP) workflows to obtain whole slide image (WSI) files for diagnostic purposes has increased in the last few years. The increasing performance of technical components and the Food and Drug Administration (FDA) approval of systems for primary diagnosis led to increased interest in applying DP workflows. However, despite this revolutionary transition, real-world data suggest that a fully digital approach to histological workflow has been implemented in only a minority of pathology laboratories.
The objective of this study is to facilitate the implementation of DP workflows in pathology laboratories, helping those involved in this process of transformation with: (a) how to identify the scope and the boundaries of the DP transformation; (b) how to introduce automation to reduce errors; (c) how to introduce appropriate quality control to guarantee the safety of the process; and (d) addressing the hardware and software needed to implement DP systems inside the pathology laboratory. The European Society of Digital and Integrative Pathology (ESDIP) provided consensus-based recommendations developed through discussion among members of the broader scientific committee. The recommendations are thus based on the expertise of panel members and on the agreement obtained after virtual meetings. Prior to publication, the recommendations were reviewed by members of the ESDIP Board. The recommendations comprehensively cover every step of the implementation of a digital workflow in the anatomic pathology department, emphasizing the importance of interoperability, automation, and tracking of the entire process before the introduction of a scanning facility. Compared to the available national and international guidelines, the present document represents a practical, handy reference for the correct implementation of a digital workflow in Europe.
Keywords: digital pathology, anatomic pathology workflow, whole slide imaging, laboratory information system
Introduction
The interest in implementing digital pathology (DP) workflows to obtain whole slide image (WSI) files for diagnostic purposes has increased in the last few years. This is in part due to the opportunities offered by WSI, e.g., telepathology and image analysis, including computational pathology tools based on artificial intelligence (AI) methods. The increasing performance of technical components and the Food and Drug Administration (FDA) approval of systems for primary diagnosis[1] led to increased interest in applying DP workflows. Moreover, in the last few years, several studies evaluating performance demonstrated the non-inferiority of WSI compared to conventional light microscopy[2][3][4] for primary histological diagnosis. This may help to alleviate concerns about the possible risk of DP-related diagnostic errors.[5] Indeed, the restrictions suffered during the COVID-19 pandemic, the reduction in the number of pathologists, and the increase in workload, along with a rising number and complexity of clinical cases, also raised the interest in DP.
Several definitions for DP have been proposed so far[6][7], a common opinion being that DP encompasses the photographic documentation of the macroscopy of the specimens (“gross pathology”), the digitization of glass slides (virtual microscopy), and telepathology. By some definitions, DP involves merely the digitization of glass slides. In this study, “DP” is significantly distanced from the reductive paradigm of only glass slide digitization, moving towards a more integrative approach that comprises interventions in all stations of work in the pathology laboratory, introducing and supporting innovation. DP implicitly consists of all the associated technologies to allow improvements and innovations in workflow, including, for instance, laboratory information systems (LIS), digital dictation, dashboard and workflow management, electronic specimen labelling and tracking, and synoptic reporting tools.
The objective of this study is to facilitate the implementation of DP workflows in pathology laboratories, helping those involved in this process of transformation to: (a) identify the scope and the boundaries of the DP transformation; (b) introduce automation to reduce errors; (c) introduce appropriate quality control to guarantee the safety of the process; and (d) implement the hardware and software needed to implement DP systems inside the pathology laboratory. Since several recommendations and guidelines have already been proposed, primarily focusing on the validation of WSI for clinical purposes or on the technical environment, this paper mainly covers DP implementation and all the prerequisites for a pathology laboratory to change from an analogue to a digital workflow.[8] Considering all that has been reported about DP workflow implementation and its associated benefits, it is anticipated that this new methodology has many advantages that should be attractive and convenient for all pathology laboratories worldwide, independently of their dimension, workload, number of pathologists, or type of activity (e.g., academic/nonacademic, private/public).[6][7][9][10][11]
So far, there are several possibilities to transit and to manage “images” in a digital workflow: an LIS-based approach[12][13], a scanner vendor approach[7], or an intermediate software approach (e.g., Linköping University[14]). Independently of the type of strategy chosen, in order to switch towards a digital visualization of images (whether LIS-centric, vendor-based, or third-party software), the new system should be able to integrate every possible instrument (e.g., one or more scanners from the same or different vendors, with the possibility to manage different images from a variety of sources), preferably associated with a tracking system because of automation and innovation. The cost-effectiveness of DP has already been documented in implementation models that discuss the scope of investment, the potential return on investment, and cost-savings of DP, as well as any proposed income deriving from the adoption of WSIs.[15] Moreover, the adequate adaptation of a routine clinical workflow can finally lead to an optimization of resources (e.g., space, time, personnel, and equipment). These are intended as recommendations and suggestions for the implementation of the full DP workflow in the routine clinical practice of anatomic pathology laboratories. The introduction of a DP workflow even allows the implementation of computational pathology tools such as AI.
The following sections explain, point-by-point, the steps needed for the progressive, secure, and efficient transition into a DP workflow. Regarding cytopathology, there are several barriers that still need to be overcome for routine cytopathology to go digital and support wider adoption and sustainability. Therefore, the present study mainly focuses on histopathology and the justification (Box 1) for its transition to a DP workflow.
| Box 1. The justification of transitioning histopathology workflows to digital pathology workflows. |
| 1. Digital pathology is pathology, a holistic approach that comprehends interventions in all stations of work at the pathology laboratory, introducing innovation. 2. Digital pathology is attractive and convenient for pathology laboratories worldwide. |
Involvement of the team in the digital pathology transformation of the laboratory
The implementation of digital pathology requires a multidisciplinary approach from the very beginning. The leading team should involve in-house participants (e.g., pathologists, laboratory technicians, administrative staff) and the hospital’s IT and technical services.[6] IT services might be organized in different ways depending on the size of the department and depending on local or national policies. For example, IT services may be provided by individuals, by a separate department, or by a subcontractor. The most important thing is that these groups work together and that they form a team.
Subsequently, close collaboration with companies providing the digital pathology system and the LIS will become necessary. Especially in larger departments, digital transformation will usually be organized as a project that includes a project manager, a steering group, and different working groups. There are several ways of introducing the topic and designing the appropriate options for the laboratory at hand, and it might be useful to visit pathology departments with digital workflows to learn from their successes and failures. There are a couple of papers that share such experiences and provide valuable information.[6][7] Describing user scenarios is another method to both understand the needs of one’s own laboratory and communicate those needs to the IT and technical departments, as well as potential vendors. In addition, before starting a tender, it is helpful to gather information about suppliers and products.
To obtain a successful implementation of DP and to avoid deficiencies, the multidisciplinary team that is going to lead the “digital revolution” in each department should follow some crucial steps, as previously reported. In particular, for the correct and rapid implementation of DP in every department, it is advisable to create awareness and appropriate work conditions, incentivize participation, encourage communication among the team members, and monitor the outcomes of this revolution. This approach could help in facing the heterogeneous patterns of reactions that different actors of the team could express, including the “enthusiasts,” the “sceptics,” and the “undecided.” All the possible measures to increase the trust and involvement of pathologists should be applied to all staff members.
To establish a successful DP workflow, a thorough stakeholder analysis should be carried out, and a communication strategy should be established based on this analysis. The team must ensure that all internal stakeholders (including pathologists, laboratory personnel and administrative staff) are continuously informed from the beginning. In this setting, sharing the vision of DP with laboratory and administrative personnel, encouraging them to provide feedback, expressing potential concerns and suggestions (e.g., using frequent meetings on-site), and providing appropriate discussion during all phases of the deployment will facilitate a safe and effective implementation. The team must be aware that DP should be perceived as an integral part of the laboratory workflow rather than an “add-on.”[6] The contingent situation due to the COVID-19 pandemic can be further leveraged to boost the implementation of DP in the laboratories, stressing the need to maintain pathology services by making it possible for pathologists to work from home.[16]
Implementing DP as the standard laboratory practice also requires learning new technical skills to capture all the advantages of this technology. Just as significant as consulting the internal stakeholders is the involvement of IT services. IT will be crucial in many aspects of the project (e.g., handling LIS adaptations, integrations, storage, testing etc.). The involvement should start in the early phases of the transition. For example, consider conducting a laboratory office tour to establish communication with the other components of the project, using clear language. This gives your team the opportunity to understand what is expected and what is potentially achievable from your deployment, and what each professional group will be expected to contribute in terms of time and staff. Explain your ideas for future digital workflows and see what potential dependencies and solutions your IT colleagues can generate.
Optimization of resources in the DP workflow
In a fully digital laboratory, the processes and records are electronic file-based and the environment is paperless, with glass slides being substituted at the end of the workflow by WSIs. The optimization of resources—namely time, space, people and instruments—creates conditions for increased efficiency and, consequently, decreased costs. The LEAN approach represents a valuable strategy to optimize the workflow, leading to a more logical distribution of the spaces to minimize staff and specimen traffic inside the laboratory. It also allows for a more harmonic and well-planned articulation between human resources and available instruments, which results in time and cost-effectiveness. And, although it is not a strict prerequisite for adopting DP, it could further allow for better allocation of resources.[17]
This reallocation could start from a more rational disposition of the spaces or offices inside the pathology laboratory. An inefficient arrangement of the physical spaces, typical of the old, “analogue” workflow, can partly impair the smooth crosstalk among the different components of the process. Previous experiences in implementation models stress the need to analyze the pre-existing workflow before implementing DP.[6][7] A careful analysis of the pre-existing analogic workflow before the transition should consider the flow of the specimens (workstation location) in the laboratory and time intervals (hands-on and waiting times) for each workstation, verifying the information technology support and establishment of adequate quality control checkpoints. The lack of structural organization of some pathology laboratories, including the physical placement of the different workstations, may contribute negatively to the desirable, efficient crosstalk between workstations. The reorganization of such a laboratory structure with the intent to decrease unnecessary movements of the staff, and time loss, can be useful for every laboratory, independently of DP implementation. For instance, the scanning workstation should be located near the staining and mounting instruments, accelerating the production line but far from the microtome area to avoid the interference of paraffin with the scanning mechanisms. After this retrospective analysis and reorganization of the structure, the optimal choices for the automation of each workstation must be made, namely by the introduction of a reliable tracking system, and different instruments would preferably work in a coordinated fashion, connected (mono- or bi-directionally) to the LIS or laboratory information management system (LIMS).
The role and potentialities of laboratory informatics resources
Independently of the system employed to manage the WSI, pathology laboratories mainly depend on a laboratory information systems (LIS) to support their operation and, ultimately, carry out their patient care mission. For these reasons, one of the crucial points is to ensure the full integration of the systems involved in the digital transition. Although many LISs have evolved with sophisticated and more user-friendly software over the past few decades, supporting a broader range of functions, many others have not evolved, thus preventing possible integration with other technologies deployed in pathology laboratories. A modern LIS plays different roles in all phases of patient testing, including specimen and test order entry, specimen processing, and specimen tracking. They track and organize the laboratory’s workflow, mainly through event logs and histology protocols. The maintenance of such logs can follow the default configurations of the system or can be customized by each laboratory to display the most useful information. A typical example of the system’s default configuration for a log (e.g., routine histology) includes accession number, timestamp, patient and specimen data, histology protocol(s) ordered, other stains ordered, and comments about the specimen or the request.
An LIS now incorporates multiple features that, until recently, were either unavailable or required a significant customization effort to be obtained. The Association for Pathology Informatics produced a comprehensive list of basic and advanced LIS features that may be used to evaluate LIS capabilities.[18] Moreover, the next generation LIS should be able to link digital images to the respective cases appropriately. With the rising use of WSI for clinical purposes, a consensual increase in capabilities to connect and integrate WSI systems and LIS is to be expected (e.g., being able to open WSI from the LIS, log the viewed areas/magnification on all WSI, or even apply image analysis and store result data). Further advances in the development of the LIS are expected in the future, starting from the integration of more sophisticated tools to support data mining and the analysis of pathology and clinical data sets. The LIS may evolve into a multimodality “pathologist cockpit” that not only provides LIS functions but also displays pathology imaging and other medical imaging, supplies analytical tools, provides access to clinical data (e.g., through an electronic health record [EHR][19]) as well as other data sources.[20] A more recent guideline paper[21] underlined the importance of digital pathology interoperability, with a LIS being able to connect all the instruments present in the laboratory to support critical DP use cases. Moreover, increasing requests for molecular and genetic tests on pathology specimens (e.g., next-generation sequencing) impose further innovation on the LIS to integrate and optimize these data with the traditional pathology report for optimal patient management[22] in an integrative model. Finally, the transition will allow information integration from grossing, enable collaborative work, and incorporate quality control results.
Automation of workflow and tracking system
Automation and using a robust tracking system can significantly reduce errors related to handwriting transcription and misspelling that can cause specimens to be dissociated from a particular patient (“mismatching”). Automation is a “strong recommendation” emanating from these recommendations, as it can benefit both pathology laboratories using DP and those using glass slides for diagnosis. Besides the introduction of a suitable LIS or LIMS that can help monitor the instruments’ performance connected to each specimen, further automation can be introduced in the lab's workstations. This includes tracking the reagents used and tracking all the staff that were at any point involved in specimen processing by differential log-ins or scanning of individual ID codes at all workstations. Yet the possible automation of workstations obviously depends on budget, existing instruments, and the experience of the technical staff. Devices such as a robotic stainer and a cover-slipper will bring consistent slide quality, avoiding frequent re-staining and ongoing readjustments to scanning protocols. The same is true for the automation of embedding and cutting processes, for which available systems on the market appear promising. However, these are not yet widely used in practice[23], perhaps in part due to cost.
The goals of any tracking system in the laboratory are to keep the specimen automatically, correctly, and permanently labelled during the time that it circulates in the laboratory. The identification of the specimen—using labels on the containers, printed in the cassettes/paraffin blocks, printed on the glass slides and present in the WSI files—is a best practice rule that is recommended to be adopted for the use of the WSI. In this setting, the perfect compatibility (interoperability) of the instrumentation used to label and to process the specimens within the anatomic pathology laboratory, and with the other laboratories in the same institution, is crucial to avoid possible issues (e.g., blurring or shading of the labels during subsequent processing of specimens/slides). The identifiers related to the specimen, of which there are usually several (see the next section), should be managed automatically and electronically connected to the patient’s LIS entry. The integration between the tracking system and LIS with an electronic interface between the LIS and the printers is essential to maintaining continuity of identification. The link established between the asset (tissue container/cassette/block) and the LIS will help reduce errors and can be achieved by printing different data types on the assets, such as barcodes or 2D (QR) codes. These can be linked to different types of data in the LIS. Eventually, other systems with code reader compatibility will be able to read them.[24] The introduction of radiofrequency identification (RFID) technologies is also a promising method to track the assets, although cost and system integration barriers still limit their implementation.[25][26] In the case of pathology laboratories, introducing at least one barcode reader per workstation is recommended. Tracking an individual specimen with the combined use of printers and code readers accelerates the work at the microtome stations, helping histotechnologists track each block and slide, ensuring the adequate identification and concordance between the individual block and slide labels.[27]
An LIS typically offers laboratories some capability to customize the format and content of their slide labels. As will be further explained in the subsequent sections of the document, the employment of unequivocal 2D barcodes can have a multitude of applications in the proposed digital workflow, significantly reducing the operations time and error rates. The impact of such implementation can be noted starting from the accessioning phases, where the specimen is assigned its unequivocal code that will be used later during the processing and reporting steps. This can further help in the creation of tissue cassettes, in the production of tissue glass slides, in the automatic request of additional histochemical and immunohistochemical (IHC) stains, as well as in the double check that should be carried out at every checkpoint to ensure correspondence among received material, grossed specimen, embedded sample, and cut sections. This is facilitated by the additional use of barcode readers and by the implementation of newly introduced instruments to capture the cut surface directly from the paraffin block[28], which is at this point essential to guarantee a sustainable and reliable quality control process (see the next section).
Quality control program and definition of checkpoints
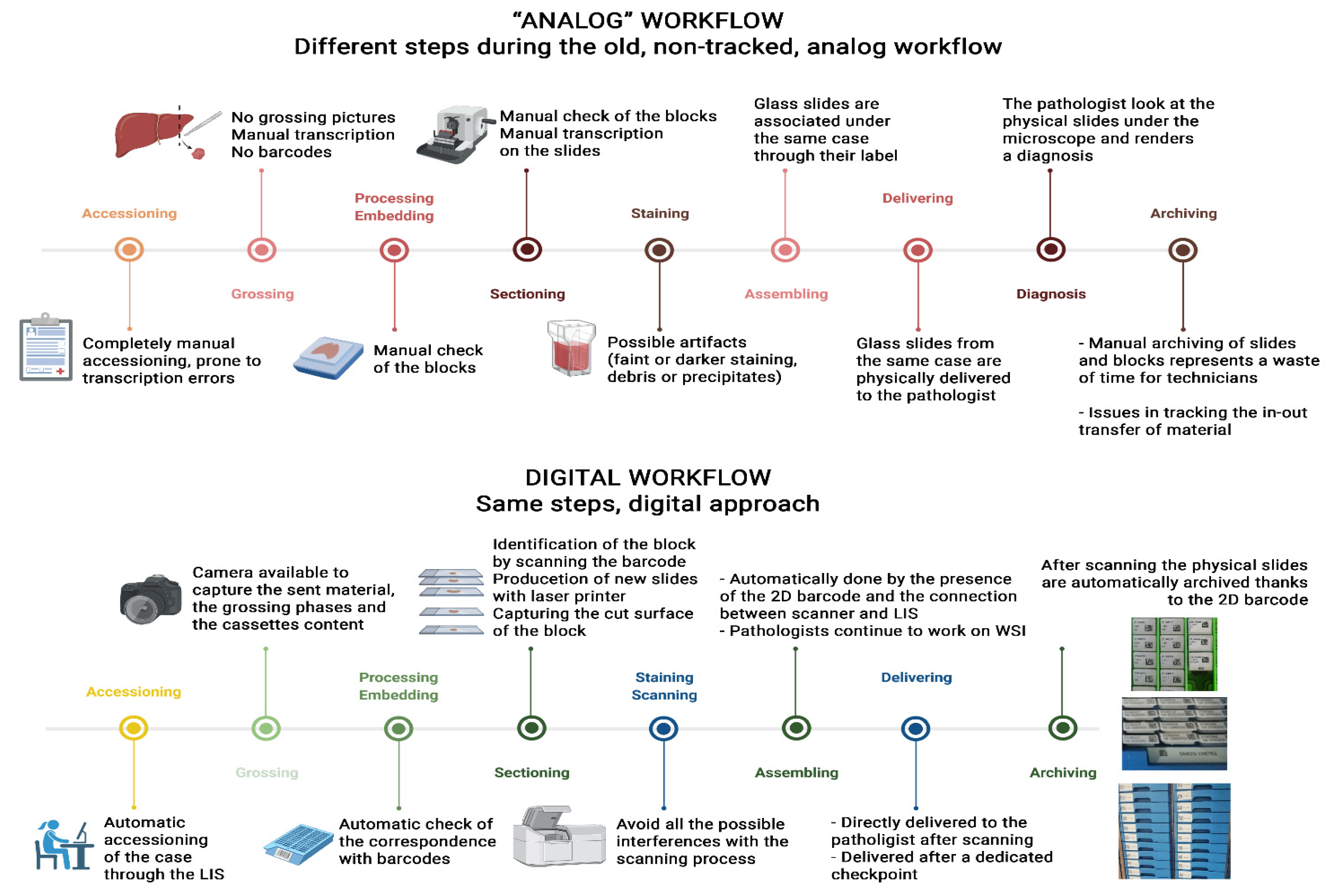
Quality control of products from a pathology laboratory is essential to guarantee that a patient receives a correct diagnosis. In Europe, the certification and accreditation of laboratories are not equally and uniformly performed across the territory. Instead, many laboratories design their own quality control program, more or less simplified, often involving only segments of specimen processing adequate to their intent. Although adopting a quality management system is not strictly required in all countries as a prerequisite for implementing DP workflow, laboratories with a robust system of quality management may find the DP workflow easier to implement as they are already aware of the critical control checkpoints through the analogue workflow. To support those laboratories that are not yet familiar with quality control programs, a detailed description of some suggested checkpoints suitable for adaptation to each laboratory are provided. The checkpoints described here derive from the need to control the performance of a new instrument in the pipeline—the scanner. They also originate from introducing new standard operative procedures (SOPs), tools, instruments, and quality control of the processes (Figure 1).
|
Simultaneously, per each workstation, some technical modifications are discussed to facilitate the scanning process and increase the quality of the WSI. We highlight that time loss within the laboratory is frequently motivated by a mismatch of specimens and poor specimen quality (either due to a pre-analytical or analytical factor). Investing in a workflow with a good quality of specimens that are easy to track decreases the time lost, considering that this loss is very difficult to estimate because it is not generally recorded.
Accessioning checkpoints
During the accessioning phase, specimens that arrive at the pathology laboratory are registered in the LIS and given a case number. Analyzing the classical analog accessioning procedures allows for a critical evaluation of the potential issues that can and do happen. Mistakes can occur in the compilation of paper requests from the submitting department or outside hospital (for internal and external cases, respectively). The staff responsible for the accessioning phase can miss discrepancies between the specimen or slide and the request, or even mismatch this pair. The manual loading of the specimen and associated patient data into the LIS can impair the link with the patient profile present in the hospital information system (HIS), generally due to an inappropriate transcription of a patient’s identification data, eventually causing a duplication of the patients’ profile, and consuming time. In a laboratory with a DP workflow, laboratory personnel have the possibility of completing these accessioning tasks automatically to minimize the risk of errors. The different identification codes (IDs) used in the various subsequent steps play a crucial role here. Similar to a pyramid or hierarchy, different types of IDs are attributed to the patient, and everything associated with this accessioning event, as follows:
- Patient ID
- C ID
- Specimen container ID (entry lab)
- Sample IDs
- Block IDs
- Slide IDs
For DP, a mechanism is needed to get required case information to the administrative department and the pathologist, including the patient ID and demographic information, a description of the specimen or sample, the clinical history, and any questions or requests for the pathologist. In the DP laboratory, the accessioning process is modified and may include some or all of the following (Table 1):
- Specimen/slides arrive in the pathology laboratory with a label containing a code (entry lab, preferentially 2D type) associated with patient and case data.
- By scanning the code on the label of the case, the administrator is able to open the digital request in the pathology LIS automatically, allowing the automatic synchronization of the information from the hospital system or creating the specific page for cases/patients coming from outside.
- A case ID for the specimen is generated.
- The case ID is then used in all sorts of sampled assets generated for that case (cassettes, new slides, special stains, digital slides).
- The administrator can take pictures of both the container and the specimen, and these photos will be attached to the case file.
- All of the documents received together with the specimen are scanned and attached to the case file or directly transmitted to the LIS digitally (e.g., via optical character recognition [OCR]).
| Table 1. Suggested checkpoints at the accessioning workstation |
| Accessioning checkpoints |
|---|
| 1. Specimens/slides are accessioned, using an order entry system, after the scanning of a code that identifies the patient/case, imports all the necessary information from the integrated HIS and opens the digital request: a procedure that introduces automation and consequent reduction of transcription errors. |
| 2. A number and the respective identification code are generated for each sample, and the identification code is used for various assets generated for that case: a procedure that allows the tracking of the sample while it is circulating in the laboratory. |
| 3. Dedicated personnel take a picture of the container and of the specimen, and those photos are attached to the case file: a procedure that documents the product entering the laboratory as well as the respective identification; this may represent an important medico-legal registry. |
| 4. The documents that may be received with the specimen are scanned and attached to the case file or directly transmitted digitally (OCR): a procedure that facilitates access to relevant information that is prevented from being lost in a workstation. |
Grossing checkpoints
After accessioning, cases are ready to be macroscopically analyzed, described, and grossed by the pathologist or trained technical staff. As this happens in accessioning, the grossing workstation may be a source of human errors. These errors may include wrong assignment of the macroscopic description and grossing of one patient in the paperwork of another patient; loss of manual transcription of specimen descriptions; deterioration of the numbers on the cassettes; and incongruences among the specimen received, grossed, and subsequently processed in the absence of step-by-step picture documentation.
As in the other workstations, through automation, the DP workflow can help reduce to a minimum the human interference needed in the grossing phase. The previously described process would be as follows (Table 2):
- The grossing operator (e.g., pathologist/resident/pathologist’s assistant) can access the case/patient file by directly scanning the code on the specimen container.
- Pictures are taken of the specimen before it is described and grossed, as well as during grossing, and finally of all tissue cassettes with slices; those images are directly linked to the case using the software integration paths between the LIS and the image capture instrument.
- The grossing operator performs a macroscopic description of the specimen through automated speech recognition systems that report the text in the appropriate section of the case/patient file using the software integrations paths between the LIS and the dictation system instrument.
- The operator can produce cassettes by using a specific printer (preferably laser printer) to assign an identification code corresponding to the particular case, as established during the accessioning, and using the software integration paths between the LIS and the printer. The cassettes and marker media should be appropriately tested to demonstrate the indelibility or impossibility of washing away or removing the identification code. The suggested code is 2D (e.g., QR code), which can include a greater character count (higher data density), require a smaller footprint, and have fewer scan and printer failures than 1D codes.
- An image of the cassette with the grossed specimen should be obtained at the bench, allowing retrieval of this at the following steps.
| Table 2. Suggested checkpoints at the grossing workstation |
| Grossing checkpoints |
|---|
| 1. Scanning the identification code on the specimen container allows for automatic access to the patient/case data, preventing transcription errors. |
| 2. The photographic documentation of the specimen as it is in the container, during grossing, and within the cassettes (for comparison to what is arrived at the embedding station) guarantees the preservation of the case features and identification. The automatic introduction of the photographs into the patient/case file at the LIS prevents mismatches and time loss. |
| 3. The macroscopic description of the specimen is dictated and converted to text through voice recognition functions of the LIS or of an instrument connected to the LIS preventing transcription errors and time loss. |
| 4. Cassettes are printed with the identification code of the sample to be tracked in subsequent workstations. |
| 5. The material inserted in the cassette during grossing can be captured to obtain retrievable pictures at the following steps. |
Grossing-to-processing and processing checkpoints
After the grossing phase, cassettes containing the specimens are ready to be processed. At this stage, further checkpoints may be needed to verify that all the cassettes generated at the grossing workstation are present in the rack to be processed. This double-check is still routinely and primarily done manually in most pathology laboratories. In a DP workflow, this task may be carried out by scanning the codes printed in the cassettes of the rack before they are processed, and checking if all the produced cassettes are submitted to the subsequent phase, integrating the information in the LIS. During the processing phase, both the instruments and programs used should be preferentially recorded through the employment of an appropriately integrated LIS, allowing for tracking the specimens/cases at this workstation. This system can be further deployed to track the usage of reagents for processing, helping in the safe disposal of these reagents. Moreover, the integration with the LIS can further help aggregate specimens and cassettes in different racks based on their processing time and scanner time/protocol requirements (e.g., fast vs. standard processing), or even separate specimens processed in different instruments.
Embedding checkpoints
Once the processed specimen inside the cassettes have arrived at the embedding room, operators (technicians) should be able to access the pictures taken during the grossing phase by simply scanning the barcode (Table 2). This will allow them to compare them with the content of cassettes after processing, checking their correspondence to rule out the loss of biological material. Correct embedding may prevent the creation of poor-quality virtual slides. One of the possible issues during the scanning phase is represented by the presence of large fragments, which are more prone to be hydrated during the processing steps and thus more complicated to be captured by the scanner. To address this problem, the fragments should be reduced during the grossing phase, and the embedding checkpoint is essential to control this point. Similarly, tissue fragments well oriented, levelled, and close to each other in paraffin, may constitute good substrates for better-quality glass slides. If the extracted sample to be analyzed is too large to be fitted in a regular glass slide, the recent introduction of dedicated scanners for “macro” glass slides provides the possibility of this solution directly from the grossing room.[29]
Sectioning checkpoints
The sectioning workstation is a time-consuming phase of the laboratory flow where errors are frequent. Here, automation can facilitate the technician’s work, bringing increased control and fewer errors, and resulting in less time spent. The sectioning workstation is complex and requires the rapid manipulation of specimens and instruments in a consecutive way. The introduction of a slide printer, a code reader, a desktop interface, and similar devices can be initially perceived as a further complication of this step.
Checkpoints can be installed at this workstation depending on the laboratory’s needs and may prevent important errors (Table 3). Moreover, the employment of a slide printer (e.g., laser) at the sectioning station connected to the tracking system should be preferred over “classic” handwritten or printed labels in order to reduce the risk of mismatches. The LIS should also be the source of all the information regarding the types of stains to be performed (i.e., IHC or “special” tinctorial stains) from a specific block. Moreover, the introduction of dedicated instruments to capture the cut surface of each paraffin block[28] could represent an additional checkpoint, helping to further reduce tissue inconsistencies among the blocks and the final glass/virtual slides. The sectioning process should follow the highest operative standards to minimize errors and poor quality in the subsequent scanning phase. Indeed, the irregular thickness of a tissue section, and the presence of holes or scratches and debris erroneously collected from the bath, can impair the correct scan of the final glass slide product. The same is true for sections located at the edges of the slides, which may pass undetected by the scanner. Thus, the sections should be thin enough during the cutting phase and preferentially located in the middle of the physical glass slides to ensure the most appropriate scanning quality. Automatic microtomes may contribute to decreased tissue thickness variations.
| Table 3. Suggested checkpoints at the sectioning workstation |
| Sectioning checkpoints |
|---|
| 1. The code printed on the paraffin block may be scanned to open the case file through the integrated LIS, preventing transcription errors. |
| 2. The technician can check how many and which kinds of slides are needed for each block directly on the LIS. |
| 3. For each paraffin block, one or more printed glass slides are then generated through a dedicated printer, with all the slides having a unique identifier. |
| 4. After sectioning, each paraffin block may be photographed to assess whether all the material emerged on the glass slide/WSI. |
| 5. The sectioning phase should follow high operative standards, reducing the risk of artifacts that can impair the scanning phase. |
Staining and mounting checkpoints
Once in the staining workstation, the slides produced in the digital workflow are identified through their code to define which staining protocol they should follow, as per internal LIS prerecorded indications, using automated staining platforms. As in the previous step, the staining process should follow the highest qualitative standards to reduce possible modifications that can interfere with the scanning phase (faint or darker staining, debris/precipitates). For this purpose, implementing an internal checkpoint with daily controls and/or external quality control can help assess the quality of stained slides.[30] Automating the staining may contribute to a stable result, allowing the design of a scanning protocol applicable to most of the slides, avoiding restaining and rescanning slides. The production of consistent staining with a clean background is relevant because it decreases the size of the produced digital slides. A final word is needed to address the mounting process and respective automation. To minimize the interference of the mounting medium in the scanning process, the laboratory must select the mounter, the coverslip type, and respective mounting medium to be used in all sorts of glass slides so that the scanner can be calibrated accordingly. Before the scanning phase, it is of paramount importance to check whether the slide is in an adequate state for scanning. After the staining/cover-slipping phase, it should be dry to prevent scanning problems (e.g., stitching, blurring, out of focus areas). Moreover, the scanning phase can be either affected by the different positions of the coverslips, leading to a misalignment of the slides in the rack. Differences in the type of coverslip can be responsible for a high rate of WSIs being out of focus. The use of automatic mounters obviates variations in the quality of the mounting and prevents errors if an adequate revision of the mounter is provided.
Correcting assigning of the WSI to the case checkpoints
This topic is discussed further in the next section on scanning.
Archiving checkpoints
After the sectioning and scanning phases, blocks and slides can be appropriately archived to be retrieved whenever is necessary. This task has been historically performed manually by operators (technicians or laboratory assistants), leading to loss and misplacement of blocks/slides, with obvious medico-legal consequences. Moreover, the wide practice of consulting archival material by all the laboratory workers, including residents and students for didactic purposes, can further complicate the correct positioning of these specimens. Based on these observations, full integration with the LIS and the presence of unique identifiers, both on the blocks and glass slides, allow for a more procedural yet automated archiving of all the biological material, as well as its safe and unbiased retrieval if needed when, for example, a request of external consultation arrives. (For archiving of the WSI, please refer to the data retention policy, discussed later in the section on "Validation of WSI for clinical use.")
Scanner for slide digitization
This section contains some considerations and recommendations for selecting and managing the most appropriate digital slide scanner, given a set or requirements for the scanning phase (Table 4). As in other medical specialties, which have been dramatically changed by the introduction of a wide variety of digital devices for routine daily work[31], it is not the focus of the present recommendations to draw a meticulous review of the technical characteristics of a scanner, since several studies have already been published on this subject.[32][33]
| Table 4. Recommendations for the scanning phase |
| Scanning checkpoints |
|---|
| 1. At any given time, two scanners digitize twice the number of slides compared to a single scanner, and three scanners triple this (e.g., for a caseload of 300 slides per day, employing three scanners with 100-slide capacity could be better than using a single scanner with a 300-slide capacity). |
| 2. It is advisable to scan during the daytime, with the lab personnel present to solve unexpected problems. |
| 3. Scanning sessions during the night might be problematic in some already established workflows; thus, if there are problems with the scanning process, it might be better to avoid scanning after working hours. |
| 4. A single-scanner approach is not recommended when contemplating a daily routine diagnostic workflow. |
| 5. Consider the possibility of a continuous loading and eventual prioritization of a batch of slides. |
The most appropriate scanner should be selected based on the needs of the specific laboratory (e.g., primary diagnosis, consultation, education, and research). The following section focuses on the possible impact of such a choice on DP workflow implementation. According to the LEAN approach, as discussed earlier, the positioning of the scanners should follow the logic of an automated workflow and thus be placed as close as possible to the staining and cover-slipping stations, making their implementation in the entire process easier and smoother.[6][7]
The transition to digital pathology also includes choosing the most appropriate types and numbers of scanners for the lab. Although it is highly dependent on the needs of each specific laboratory, one way to estimate the number of scanners is to review previous DP experiences.[6][7] In this context, each department should be aware of the expected application of the scanners, the total time required for the scanning process, and the time that can be dedicated to this part of the workflow. Some formulas to calculate the numbers of scanners needed in the lab have been proposed.[6][7]
However, many variables must be considered when calculating the number of scanners required to digitize the entire slide volume within the same workday, thus not interfering with the turn-around time (TAT). These variables are limited by the technical specifications of the scanners and their related informatics networks (including bandwidth and switches) and the type and location of storage, together with the existing workflow within the lab (i.e., availability of personnel at all times of the day). One of the possible pitfalls in calculating the actual scanning time per slide/batch, and thus the number of scanners required per lab, could be represented by the reported scanning times by each vendor, generally calculated on a specimen tissue of 1.5 cm × 1.5 cm in size and with a local storage solution. However, this is far away from the routine practice of an anatomic pathology laboratory that must accommodate very small pieces of tissue (e.g., biopsies) as well as large surgical specimens, and that may even have the possibility of storing the WSI remotely or in the cloud. Moreover, since the implementation of scanners should not impact the existing workflow and eventually lead to its improvement, there is a need to evaluate a continuous loading capability to preserve the same or similar workloads over time compared to the conventional analogue counterpart. This should be coupled with the possibility of prioritizing a specific batch of slides.
A few additional comments are needed at this point. Broadly speaking, scanning during working hours should be preferred for practical and logistical reasons. If there are problems with the scanning process, it might be better to avoid scanning after working hours. For example, it has been reported that the mean scanning time in a routine environment is about six minutes for scanning a slide at an equivalent of 40 × magnification.[34] Therefore, it takes about four hours for one rack of 40 slides, and up to 40 hours to digitize all of the slides that fit inside the scanner (using an AT2, Leica Biosystems, Nussloch, Germany). However, it is well known that the scanning process may stop for several reasons, including sticky glass, connection problems, or software and hardware problems. The result may be an incomplete digitization of slides, with a consequent interruption of routine workflow in the subsequent morning. Based on the previous observations, and since the scanning process should be a continuous workflow in the lab, scanning during the day should be preferred to the overnight approach. This could enable lab personnel to react to the possible technical issues mentioned above. This could even lead to modifications in other parts of the pathology workflow to adapt routine specimen processing to the loading schedules required by the scanners.
In this setting, the laboratory can choose to switch from bulk production of slides at the end of the day to a more continuous production of derived samples. Once the number of scanners needed and the required scanning time has been defined, the laboratory should verify whether the number of working operators employed in the department is sufficient to run the instruments for the specified length of time. Otherwise, the calculation of the necessary personnel is required, considering both 1. the scanning process and 2. any virtual slide quality control. The scanning process mainly consists of loading/unloading slides in the scanner and taking snapshots to ensure that the instrument captures all the material on the glass. On the other hand, the quality control phase is equally important and may be time-consuming, encompassing all the quality check procedures of the final WSI and related data.
The points discussed above pertain to “regular” scanners for bright field microscopy. Other “special” scanners exist, e.g., those for dark field microscopy (immunofluorescence and fluorescence in-situ hybridization [FISH]), as well as those for whole mount slides (macro slides). Because of their highly specific fields of application[35], they are not the object of these recommendations.
Validation of WSI for clinical use
References
- ↑ Evans, Andrew J.; Bauer, Thomas W.; Bui, Marilyn M.; Cornish, Toby C.; Duncan, Helena; Glassy, Eric F.; Hipp, Jason; McGee, Robert S. et al. (1 November 2018). "US Food and Drug Administration Approval of Whole Slide Imaging for Primary Diagnosis: A Key Milestone Is Reached and New Questions Are Raised" (in en). Archives of Pathology & Laboratory Medicine 142 (11): 1383–1387. doi:10.5858/arpa.2017-0496-CP. ISSN 0003-9985. http://meridian.allenpress.com/aplm/article/142/11/1383/102979/US-Food-and-Drug-Administration-Approval-of-Whole.
- ↑ Snead, David R. J.; Tsang, Yee-Wah; Meskiri, Aisha; Kimani, Peter K.; Crossman, Richard; Rajpoot, Nasir M.; Blessing, Elaine; Chen, Klaus et al. (2016). "Validation of digital pathology imaging for primary histopathological diagnosis" (in en). Histopathology 68 (7): 1063–1072. doi:10.1111/his.12879. ISSN 1365-2559. https://onlinelibrary.wiley.com/doi/abs/10.1111/his.12879.
- ↑ Goacher, Edward; Randell, Rebecca; Williams, Bethany; Treanor, Darren (1 January 2017). "The Diagnostic Concordance of Whole Slide Imaging and Light Microscopy: A Systematic Review" (in en). Archives of Pathology & Laboratory Medicine 141 (1): 151–161. doi:10.5858/arpa.2016-0025-RA. ISSN 0003-9985. http://meridian.allenpress.com/aplm/article/141/1/151/65950/The-Diagnostic-Concordance-of-Whole-Slide-Imaging.
- ↑ Mukhopadhyay, Sanjay; Feldman, Michael D.; Abels, Esther; Ashfaq, Raheela; Beltaifa, Senda; Cacciabeve, Nicolas G.; Cathro, Helen P.; Cheng, Liang et al. (1 January 2018). "Whole Slide Imaging Versus Microscopy for Primary Diagnosis in Surgical Pathology: A Multicenter Blinded Randomized Noninferiority Study of 1992 Cases (Pivotal Study)" (in en). American Journal of Surgical Pathology 42 (1): 39–52. doi:10.1097/PAS.0000000000000948. ISSN 0147-5185. PMC PMC5737464. PMID 28961557. https://journals.lww.com/00000478-201801000-00006.
- ↑ Evans, Andrew J.; Salama, Mohamed E.; Henricks, Walter H.; Pantanowitz, Liron (1 July 2017). "Implementation of Whole Slide Imaging for Clinical Purposes: Issues to Consider From the Perspective of Early Adopters" (in en). Archives of Pathology & Laboratory Medicine 141 (7): 944–959. doi:10.5858/arpa.2016-0074-OA. ISSN 0003-9985. http://meridian.allenpress.com/aplm/article/141/7/944/65708/Implementation-of-Whole-Slide-Imaging-for-Clinical.
- ↑ 6.0 6.1 6.2 6.3 6.4 6.5 6.6 6.7 6.8 Treanor, D.; Williams, B.; Hussain, B. et al. (July 2018). "The Leeds Guide to Digital Pathology" (PDF). University of Leeds. https://www.virtualpathology.leeds.ac.uk/research/clinical/docs/2018/pdfs/18778_Leeds%20Guide%20to%20Digital%20Pathology_Brochure_A4_final_hi.pdf. Retrieved 10 November 2021.
- ↑ 7.0 7.1 7.2 7.3 7.4 7.5 7.6 7.7 LabPON Laboratorium Pathologie Oost-Nederland (October 2016). "How to Go Digital in Pathology" (PDF). LabPON Laboratorium Pathologie Oost-Nederland. https://www.usa.philips.com/c-dam/b2bhc/us/landing-pages/pdxus/how-to-go-digital-in-pathology.pdf. Retrieved 10 November 2021.
- ↑ Retamero, Juan Antonio; Aneiros-Fernandez, Jose; del Moral, Raimundo G. (1 February 2020). "Complete Digital Pathology for Routine Histopathology Diagnosis in a Multicenter Hospital Network" (in en). Archives of Pathology & Laboratory Medicine 144 (2): 221–228. doi:10.5858/arpa.2018-0541-OA. ISSN 0003-9985. http://meridian.allenpress.com/aplm/article/144/2/221/433661/Complete-Digital-Pathology-for-Routine.
- ↑ Fraggetta, Filippo; Garozzo, Salvatore; Zannoni, GianFranco; Pantanowitz, Liron; Rossi, EstherDiana (2017). "Routine digital pathology workflow: The Catania experience" (in en). Journal of Pathology Informatics 8 (1): 51. doi:10.4103/jpi.jpi_58_17. ISSN 2153-3539. PMC PMC5760840. PMID 29416914. http://www.jpathinformatics.org/text.asp?2017/8/1/51/221132.
- ↑ Fraggetta, Filippo; Caputo, Alessandro; Guglielmino, Rosa; Pellegrino, Maria Giovanna; Runza, Giampaolo; L'Imperio, Vincenzo (16 October 2021). "A Survival Guide for the Rapid Transition to a Fully Digital Workflow: The “Caltagirone Example”" (in en). Diagnostics 11 (10): 1916. doi:10.3390/diagnostics11101916. ISSN 2075-4418. PMC PMC8534326. PMID 34679614. https://www.mdpi.com/2075-4418/11/10/1916.
- ↑ Eloy, Catarina; Vale, João; Curado, Mónica; Polónia, António; Campelos, Sofia; Caramelo, Ana; Sousa, Rui; Sobrinho-Simões, Manuel (15 November 2021). "Digital Pathology Workflow Implementation at IPATIMUP" (in en). Diagnostics 11 (11): 2111. doi:10.3390/diagnostics11112111. ISSN 2075-4418. PMC PMC8620597. PMID 34829458. https://www.mdpi.com/2075-4418/11/11/2111.
- ↑ Sinard, John H.; Castellani, William J.; Wilkerson, Myra L.; Henricks, Walter H. (1 March 2015). "Stand-alone Laboratory Information Systems Versus Laboratory Modules Incorporated in the Electronic Health Record" (in en). Archives of Pathology & Laboratory Medicine 139 (3): 311–318. doi:10.5858/arpa.2013-0711-SO. ISSN 1543-2165. http://meridian.allenpress.com/aplm/article/139/3/311/193668/Standalone-Laboratory-Information-Systems-Versus.
- ↑ Sepulveda, Jorge L.; Young, Donald S. (1 August 2013). "The Ideal Laboratory Information System" (in en). Archives of Pathology & Laboratory Medicine 137 (8): 1129–1140. doi:10.5858/arpa.2012-0362-RA. ISSN 1543-2165. http://meridian.allenpress.com/aplm/article/137/8/1129/65418/The-Ideal-Laboratory-Information-System.
- ↑ Asa, SylviaL; Bodén, AnnaC; Treanor, Darren; Jarkman, Sofia; Lundström, Claes; Pantanowitz, Liron (2019). "2020 vision of digital pathology in action" (in en). Journal of Pathology Informatics 10 (1): 27. doi:10.4103/jpi.jpi_31_19. ISSN 2153-3539. PMC PMC6704755. PMID 31516758. http://www.jpathinformatics.org/text.asp?2019/10/1/27/264400.
- ↑ Lujan, Giovanni; Quigley, JenniferC; Hartman, Douglas; Parwani, Anil; Roehmholdt, Brian; Meter, BryanVan; Ardon, Orly; Hanna, MatthewG et al. (2021). "Dissecting the business case for adoption and implementation of digital pathology: A white paper from the digital pathology association" (in en). Journal of Pathology Informatics 12 (1): 17. doi:10.4103/jpi.jpi_67_20. ISSN 2153-3539. PMC PMC8240548. PMID 34221633. http://www.jpathinformatics.org/text.asp?2021/12/1/17/313004.
- ↑ Hanna, Matthew G.; Reuter, Victor E.; Ardon, Orly; Kim, David; Sirintrapun, Sahussapont Joseph; Schüffler, Peter J.; Busam, Klaus J.; Sauter, Jennifer L. et al. (1 November 2020). "Validation of a digital pathology system including remote review during the COVID-19 pandemic" (in en). Modern Pathology 33 (11): 2115–2127. doi:10.1038/s41379-020-0601-5. ISSN 0893-3952. PMC PMC7306935. PMID 32572154. http://www.nature.com/articles/s41379-020-0601-5.
- ↑ Zarbo, Richard J. (1 September 2012). "Creating and Sustaining a Lean Culture of Continuous Process Improvement" (in en). American Journal of Clinical Pathology 138 (3): 321–326. doi:10.1309/AJCP2QY1XGKTSNQF. ISSN 0002-9173. https://academic.oup.com/ajcp/article-lookup/doi/10.1309/AJCP2QY1XGKTSNQF.
- ↑ Tuthill, JMark; Friedman, BruceA; Splitz, Andrew; Balis, UlyssesJ (2014). "The laboratory information system functionality assessment tool: Ensuring optimal software support for your laboratory" (in en). Journal of Pathology Informatics 5 (1): 7. doi:10.4103/2153-3539.127819. ISSN 2153-3539. PMC PMC3986538. PMID 24741466. http://www.jpathinformatics.org/text.asp?2014/5/1/7/127819.
- ↑ Petrides, Athena K.; Bixho, Ida; Goonan, Ellen M.; Bates, David W.; Shaykevich, Shimon; Lipsitz, Stuart R.; Landman, Adam B.; Tanasijevic, Milenko J. et al. (1 March 2017). "The Benefits and Challenges of an Interfaced Electronic Health Record and Laboratory Information System: Effects on Laboratory Processes" (in en). Archives of Pathology & Laboratory Medicine 141 (3): 410–417. doi:10.5858/arpa.2016-0146-OA. ISSN 0003-9985. http://meridian.allenpress.com/aplm/article/141/3/410/65705/The-Benefits-and-Challenges-of-an-Interfaced.
- ↑ Krupinski, ElizabethA (2010). "Optimizing the pathology workstation "cockpit": Challenges and solutions" (in en). Journal of Pathology Informatics 1 (1): 19. doi:10.4103/2153-3539.70708. ISSN 2153-3539. PMC PMC2956171. PMID 21031008. http://www.jpathinformatics.org/text.asp?2010/1/1/19/70708.
- ↑ Dash, RajeshC; Jones, Nicholas; Merrick, Riki; Haroske, Gunter; Harrison, James; Sayers, Craig; Haarselhorst, Nick; Wintell, Mikael et al. (2021). "Integrating the health-care enterprise pathology and laboratory medicine guideline for digital pathology interoperability" (in en). Journal of Pathology Informatics 12 (1): 16. doi:10.4103/jpi.jpi_98_20. ISSN 2153-3539. PMC PMC8240547. PMID 34221632. http://www.jpathinformatics.org/text.asp?2021/12/1/16/311870.
- ↑ Roy, Somak; Pfeifer, John D.; LaFramboise, William A.; Pantanowitz, Liron (1 September 2016). "Molecular digital pathology: progress and potential of exchanging molecular data" (in en). Expert Review of Molecular Diagnostics 16 (9): 941–947. doi:10.1080/14737159.2016.1206472. ISSN 1473-7159. https://www.tandfonline.com/doi/full/10.1080/14737159.2016.1206472.
- ↑ Phelan, Sine M (2014). "Impact of the introduction of a novel automated embedding system on quality in a university hospital histopathology department" (in en). Journal of Histology and Histopathology 1 (1): 3. doi:10.7243/2055-091X-1-3. ISSN 2055-091X. http://www.hoajonline.com/histology/2055-091X/1/3.
- ↑ Hanna, Matthew G.; Pantanowitz, Liron (1 March 2016). "Bar Coding and Tracking in Pathology". Clinics in Laboratory Medicine 36 (1): 13–30. doi:10.1016/j.cll.2015.09.003. ISSN 1557-9832. PMID 26851661. https://pubmed.ncbi.nlm.nih.gov/26851661.
- ↑ Bostwick, David G. (1 October 2013). "Radiofrequency identification specimen tracking in anatomical pathology: pilot study of 1067 consecutive prostate biopsies". Annals of Diagnostic Pathology 17 (5): 391–402. doi:10.1016/j.anndiagpath.2013.04.007. ISSN 1532-8198. PMID 23796559. https://pubmed.ncbi.nlm.nih.gov/23796559.
- ↑ Lou, Jerry J.; Andrechak, Gary; Riben, Michael; Yong, William H. (2011). "A review of radio frequency identification technology for the anatomic pathology or biorepository laboratory: Much promise, some progress, and more work needed". Journal of Pathology Informatics 2: 34. doi:10.4103/2153-3539.83738. ISSN 2153-3539. PMC 3162748. PMID 21886890. https://pubmed.ncbi.nlm.nih.gov/21886890.
- ↑ Snyder, Susan R.; Favoretto, Alessandra M.; Derzon, James H.; Christenson, Robert H.; Kahn, Stephen E.; Shaw, Colleen S.; Baetz, Rich Ann; Mass, Diana et al. (1 September 2012). "Effectiveness of barcoding for reducing patient specimen and laboratory testing identification errors: A Laboratory Medicine Best Practices systematic review and meta-analysis" (in en). Clinical Biochemistry 45 (13-14): 988–998. doi:10.1016/j.clinbiochem.2012.06.019. PMC PMC4518452. PMID 22750145. https://linkinghub.elsevier.com/retrieve/pii/S0009912012003232.
- ↑ 28.0 28.1 L'Imperio, Vincenzo; Gibilisco, Fabio; Fraggetta, Filippo (2021). "What is Essential is (No More) Invisible to the Eyes: The Introduction of BlocDoc in the Digital Pathology Workflow". Journal of Pathology Informatics 12: 32. doi:10.4103/jpi.jpi_35_21. ISSN 2229-5089. PMC 8529340. PMID 34760329. https://pubmed.ncbi.nlm.nih.gov/34760329.
- ↑ Pantanowitz, Liron; Farahani, Navid; Parwani, Anil (1 June 2015). "Whole slide imaging in pathology: advantages, limitations, and emerging perspectives" (in en). Pathology and Laboratory Medicine International: 23–33. doi:10.2147/PLMI.S59826. ISSN 1179-2698. http://www.dovepress.com/whole-slide-imaging-in-pathology-advantages-limitations-and-emerging-p-peer-reviewed-article-PLMI.
- ↑ Janowczyk, Andrew; Zuo, Ren; Gilmore, Hannah; Feldman, Michael; Madabhushi, Anant (1 December 2019). "HistoQC: An Open-Source Quality Control Tool for Digital Pathology Slides" (in en). JCO Clinical Cancer Informatics 3: 1–7. doi:10.1200/CCI.18.00157. ISSN 2473-4276. PMC PMC6552675. PMID 30990737. https://ascopubs.org/doi/10.1200/CCI.18.00157.
- ↑ Ferrini, Francesco; Sannino, Gianpaolo; Chiola, Carlo; Capparé, Paolo; Gastaldi, Giorgio; Gherlone, Enrico (14 February 2019). "Influence of Intra-Oral Scanner (I.O.S.) on The Marginal Accuracy of CAD/CAM Single Crowns" (in en). International Journal of Environmental Research and Public Health 16 (4): 544. doi:10.3390/ijerph16040544. ISSN 1660-4601. PMC PMC6406818. PMID 30769768. http://www.mdpi.com/1660-4601/16/4/544.
- ↑ Hufnagl, Peter; Zwönitzer, Ralf; Haroske, Gunter (8 September 2018). "Guidelines Digital Pathology for Diagnosis on (and Reports of) Digital Images Version 1.0 Bundesverband deutscher Pathologen e.V. (Federal Association of German Pathologist)" (in en). Diagnostic Pathology 4 (1): 266. doi:10.17629/WWW.DIAGNOSTICPATHOLOGY.EU-2018-4:266. http://www.diagnosticpathology.eu/content/index.php/dpath/article/view/266.
- ↑ Cross, S.; Furness, P.; Igali, L. et al. (January 2018). "Best practice recommendations for implementing digital pathology" (PDF). The Royal College of Pathologists. https://www.rcpath.org/uploads/assets/f465d1b3-797b-4297-b7fedc00b4d77e51/Best-practice-recommendations-for-implementing-digital-pathology.pdf. Retrieved 10 November 2021.
- ↑ Hanna, Matthew G.; Reuter, Victor E.; Hameed, Meera R.; Tan, Lee K.; Chiang, Sarah; Sigel, Carlie; Hollmann, Travis; Giri, Dilip et al. (1 July 2019). "Whole slide imaging equivalency and efficiency study: experience at a large academic center" (in en). Modern Pathology 32 (7): 916–928. doi:10.1038/s41379-019-0205-0. ISSN 0893-3952. http://www.nature.com/articles/s41379-019-0205-0.
- ↑ L’Imperio, Vincenzo; Brambilla, Virginia; Cazzaniga, Giorgio; Ferrario, Franco; Nebuloni, Manuela; Pagni, Fabio (1 June 2021). "Digital pathology for the routine diagnosis of renal diseases: a standard model" (in en). Journal of Nephrology 34 (3): 681–688. doi:10.1007/s40620-020-00805-1. ISSN 1121-8428. PMC PMC8192318. PMID 32683656. https://link.springer.com/10.1007/s40620-020-00805-1.
Notes
This presentation is faithful to the original, with only a few minor changes to presentation, spelling, and grammar. In some cases important information was missing from the references, and that information was added.