Difference between revisions of "Journal:Informatics-driven quality improvement in the modern histology lab"
Shawndouglas (talk | contribs) (Saving and adding more.) |
Shawndouglas (talk | contribs) (Saving and adding more.) |
||
| Line 47: | Line 47: | ||
[[File:Fig1 Seifert JAMIAOpen20 3.png| | [[File:Fig1 Seifert JAMIAOpen20 3.png|1300px]] | ||
{{clear}} | {{clear}} | ||
{| | {| | ||
| STYLE="vertical-align:top;"| | | STYLE="vertical-align:top;"| | ||
{| border="0" cellpadding="5" cellspacing="0" width=" | {| border="0" cellpadding="5" cellspacing="0" width="1300px" | ||
|- | |- | ||
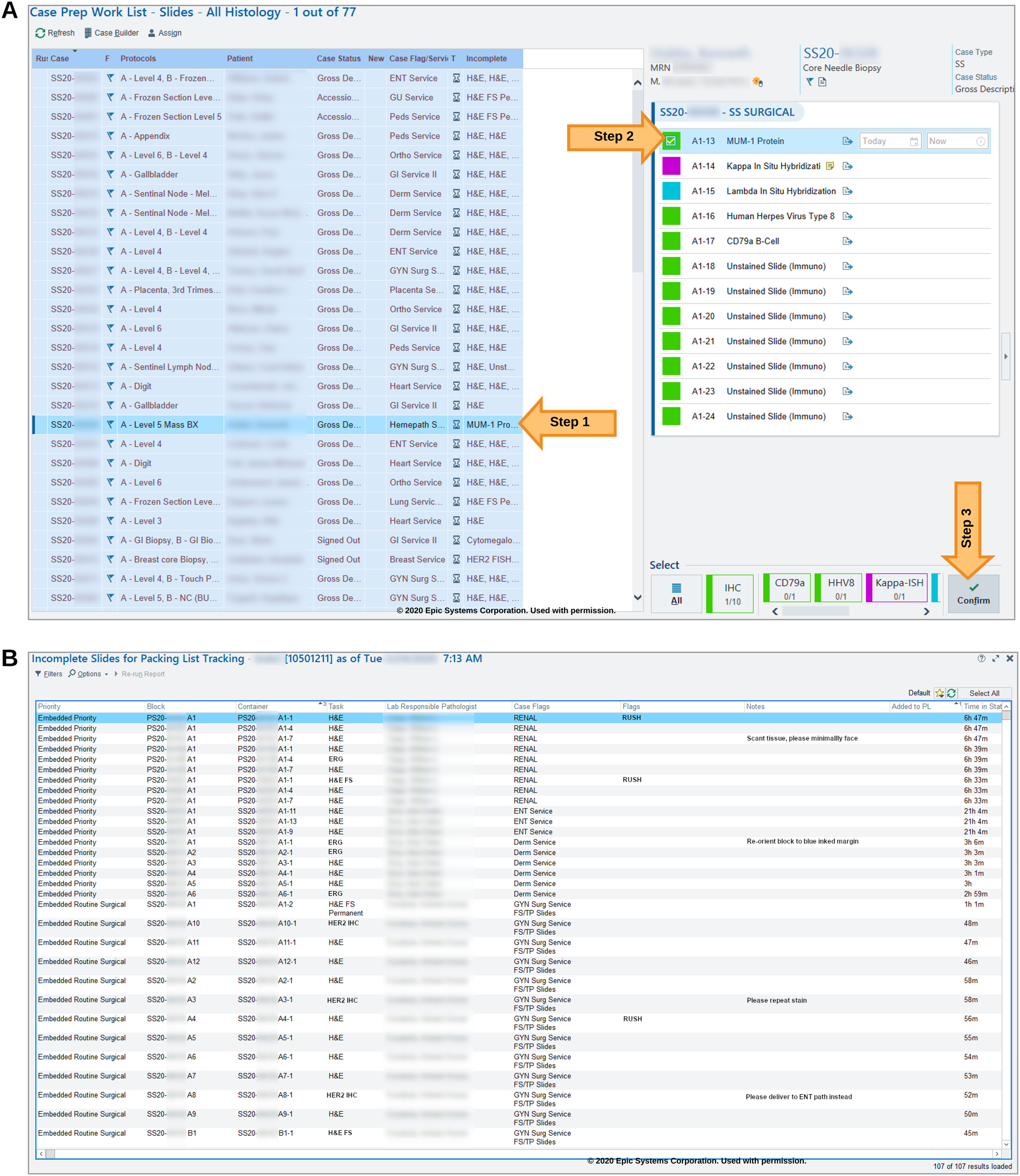
| style="background-color:white; padding-left:10px; padding-right:10px;"| <blockquote>'''Figure 1.''' ('''A''') The case-prep work list organizes pending histology tasks by case with a truncated list, the “Incomplete” column, to show the actual pending task types. Specific tasks are “confirmed” on the right-hand panel. ('''B''') Our custom “status board” is displayed in the lab similar to inpatient ward status boards. Here histology tasks are listed with their pertinent information, at-a-glance.</blockquote> | | style="background-color:white; padding-left:10px; padding-right:10px;"| <blockquote>'''Figure 1.''' ('''A''') The case-prep work list organizes pending histology tasks by case with a truncated list, the “Incomplete” column, to show the actual pending task types. Specific tasks are “confirmed” on the right-hand panel. ('''B''') Our custom “status board” is displayed in the lab similar to inpatient ward status boards. Here histology tasks are listed with their pertinent information, at-a-glance.</blockquote> | ||
| Line 65: | Line 65: | ||
===Slide volume, compensation, and resident training=== | ===Slide volume, compensation, and resident training=== | ||
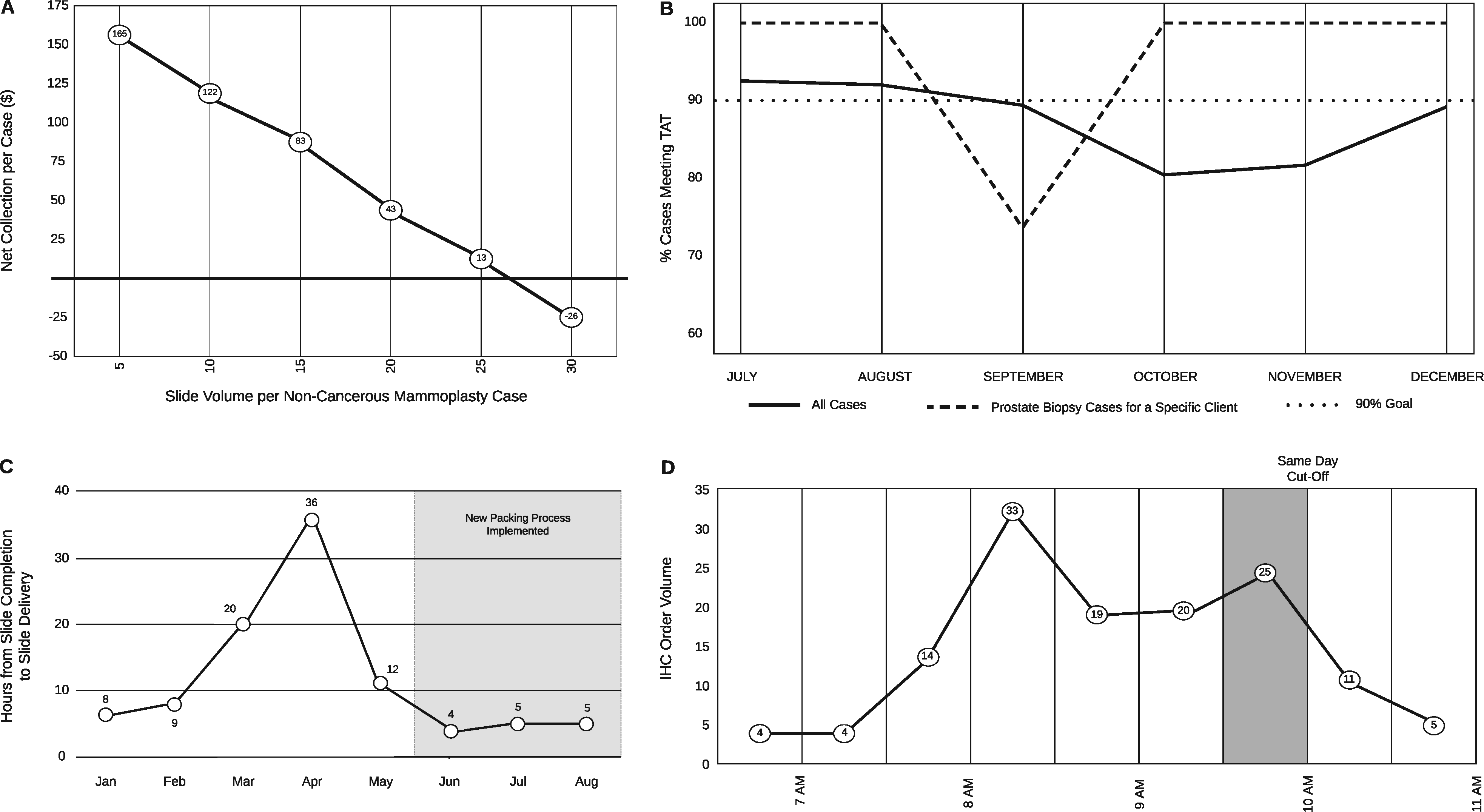
Gross tissue specimens are examined by both trained professionals (pathology assistants) as well as pathologists in training (pathology residents). Certain trainee mistakes may be overlooked by mentors and staff. Routine lab volume reporting failed to identify an increase in block volumes from cases prepared by grossing-room trainees. Specifically, excess blocks were submitted for routine mammoplasty (non-cancerous) specimens by trainees. This spike in volume delayed the processing of these specimens and impeded other lab tasks on the days in which excess blocks were submitted. To evaluate the scope and severity of the problem, we developed a data dashboard. This helped to identify the trainees driving the issue. Additionally, these data were used in conjunction with compensation data to visualize the drop in case compensation with the submission of excess blocks (and by extension, slides) on these types of cases (Figure 2A). This visualization proved useful in trainee education and corrected the blocks-per-case levels. | |||
[[File:Fig2 Seifert JAMIAOpen20 3.png|1300px]] | |||
{{clear}} | |||
{| | |||
| STYLE="vertical-align:top;"| | |||
{| border="0" cellpadding="5" cellspacing="0" width="1300px" | |||
|- | |||
| style="background-color:white; padding-left:10px; padding-right:10px;"| <blockquote>'''Figure 2.''' This composite figure shows a rendering of data generated by our SAP Business Objects dashboards. These graphs are continuously reviewed, but, as described in their relevant sections, SAP Business Objects functionality allowed for drill-down and filtering data elements to investigate and solve various histology lab problems. ('''A''') A plot of slides per non-cancerous mammoplasty case by compensation illustrates the inverse relationship between the number of blocks submitted and the net revenue. ('''B''') Prostate biopsy specimens from a specific client (dashed line) and overall (solid line) histology TAT. ('''C''') Plot of hours from slide completion in histology to slide delivery to pathologist by month. This delay was ameliorated by changing courier procedure. ('''D''') A daily surge in IHC order volume was identified immediately prior to the 10 a.m. “same day” cutoff. This surge, and its effects on case turnaround time, assisted in lobbying for additional instrumentation.</blockquote> | |||
|- | |||
|} | |||
|} | |||
===Subspecialty-specific turnaround time investigation=== | |||
Turnaround time (TAT) is calculated from the time of specimen accessioning to the time when the final pathology report is finalized. In 2019, histology leadership was notified by Genitourinary sub-specialist pathologists that our prostate biopsy TAT was slow. This was initially misattributed to a decrease in staffing, which affected the overall histology lab TAT for September to November 2019 (see Figure 2B). The prostate subspecialty-specific drop-in TAT compliance was investigated by building a dynamic TAT reporting dashboard with the capability to filter across multiple variables (e.g., surgical specialty, specimen source, contributing clinic). Using this dashboard, we filtered the cases by prostate subspecialty and client, which revealed that the delay was not due to decreased staffing but rather an idiosyncrasy in case handling. The delayed prostate specimens exclusively belonged to a specific outpatient surgical center. The case handling error was traced to the placement of the biopsies in question in a nonstandard, overlooked location. Correction of the error led to 100 percent TAT compliance by the following month (October 2019, as shown in Figure 2B). | |||
Revision as of 23:01, 2 May 2021
| Full article title | Informatics driven quality improvement in the modern histology lab |
|---|---|
| Journal | JAMIA Open |
| Author(s) | Seifert, Robert P.; Casler, Vektra; Al Qaysi, Nada; Gothi, Shaileshbhai R.; Williams, Leah; Christensen, Patricia R.; Flax, Sherri; Chamala, Srikar |
| Author affiliation(s) | University of Florida, UF Health Medical Laboratories |
| Primary contact | schamala at ufl dot edu |
| Year published | 2020 |
| Volume and issue | 3 |
| Page(s) | 4 |
| DOI | 10.1093/jamiaopen/ooaa066 |
| ISSN | 2574-2531 |
| Distribution license | Creative Commons Attribution 4.0 International |
| Website | https://academic.oup.com/jamiaopen/article/3/4/530/6012900 |
| Download | https://academic.oup.com/jamiaopen/article-pdf/3/4/530/36625866/ooaa066.pdf (PDF) |
|
|
This article should be considered a work in progress and incomplete. Consider this article incomplete until this notice is removed. |
Abstract
Laboratory information systems (LISs) and data visualization techniques have untapped potential in anatomic pathology laboratories. The pre-built functionalities of an LIS do not address all the needs of a modern histology laboratory. For instance, “go live” is not the end of LIS customization, only the beginning. After closely evaluating various histology lab workflows, we implemented several custom data analytics dashboards and additional LIS functionalities to monitor and address weaknesses. Herein, we present our experience with LIS and data-tracking solutions that improved trainee education, slide logistics, staffing and instrumentation lobbying, and task tracking. The latter was addressed through the creation of a novel “status board” akin to those seen in inpatient wards. These use-cases can benefit other histology laboratories.
Lay summary: Histopathology is the branch of medicine that involves the gross and microscopic examination of sampled tissue to help reach a diagnosis. Histology lab workflows incorporate a multitude of automated and manual steps that require close monitoring. Data visualization is a powerful tool that can illustrate workflow trends using a graphic representation of data. This manuscript describes data visualization and data analysis techniques leveraged to address frequent pitfalls in histology laboratory workflows. This led to multiple improvements in patient safety and quality of care. Our use-case solutions, presented here, can be adapted by other histology laboratories to overcome common laboratory challenges.
Keywords: informatics, laboratory information system, quality improvement, pathology, workflow
Introduction
The microscopic examination of hematoxylin and eosin (H&E) stained slides has been the cornerstone of anatomic pathology diagnosis for over a century. Virtually every surgical specimen is processed, embedded in paraffin, cut, mounted on a slide, and stained in a histology laboratory. Anatomic pathology laboratory processes contain a multitude of technical and manual workflow steps which can be further complicated by being located offsite. Automated instruments, particularly tissue processors and stainers, have accelerated histology lab work. However, important manual tasks such as specimen grossing, tissue cassetting, embedding, cutting, mounting, and tissue examination under a microscope for quality control remain largely unautomated. If these processes are not closely monitored, the quality of patient care suffers.
Most processes in a modern histology lab are captured by an integrated laboratory information system (LIS). Data visualization is a powerful tool which can illustrate workflow trends using charts, diagrams, and tables.[1][2][3] The use of data visualization on captured histology data elements from the LIS grants the ability to monitor nearly all steps of histology lab operation. Careful upstream capture of workflow steps and their corresponding data elements in the LIS can help build robust data visualizations, leading to rapid identification of processes and their improvement.[3] This improves the accuracy and timely reporting of the final pathology diagnosis, which directly affects patient care and compensation.
Our institution, the University of Florida, serves a large, roughly 1000-bed tertiary care hospital with multiple surgical subspecialties available. Diagnoses range from mundane to extraordinarily rare. Our histology laboratory also acts as an outreach lab for a number of regional clinics and is geographically separated from our main hospital and anatomic pathology offices. Our pathology department uses Beaker (Epic Systems Corporation, Verona, WI, USA) as our LIS. Beaker, as with other LIS platforms, makes use of 1D and 2D bar code reading for patient and specimen identification. Labs can use these to track specimen movement in exquisite detail and can be leveraged to evaluate anatomic pathology lab performance. We found such tracking to be essential given our lab’s geographical separation from the hospital and pathologists.
To our knowledge, few authors have explored data visualization and anatomic pathology workflows. Standout work from the University of Iowa[4] and Duke University[5] provided our institution with guidance during our Beaker implementation. However, those authors did not fully explore the potential of data visualization for quality improvement. Using a case-oriented format, this report demonstrates data visualization techniques, as applied to anatomic pathology workflows and may serve as a guide for others.
Encountered challenges and tailored informatics solutions
Histotechnologist status board
In Beaker, pending histology work is organized in a module called the “case-prep worklist.” A major deficiency in this module is that it is case-based and not task-based. Every line in the case-prep worklist represents one case, which can have multiple tasks (e.g., see the incomplete H&E, MUM-1, and Her2 tasks in Figure 1A). In a complex lab, histotechnologists work on dedicated sets of tasks and do not work in a case-based manner. For example, a histotechnologist may only work on biopsy H&E slides for their shift.
|
Within Beaker, pending tasks are presented as a single, concatenated and truncated string within a column (see the “Incomplete” column of Figure 1A) with no option for sorting, filtering, or expanding. Histotechnologists must click on a case in the list to view all pending tasks in a separate individual pane (see right-hand pane in Figure 1A, Steps 1 and 2). To begin work on a slide, a histotechnologist needs to mark the individual task as “confirmed” (Figure 1A, Step 3). At this point, a unique label is printed for the slide, and the task disappears from the case-prep worklist (Figure 1A). This is disadvantageous since the system considers the task to be complete at this point when, in fact, the work (technical process of slide preparation) is just beginning. Also, there is minimal flexibility in changing task parameters after it is confirmed. Specific task details, such as rush priority, as well as the tasks themselves, can be “buried” amid other information. We found the overall histotechnologist user experience for the case-prep worklist unintuitive during initial Beaker implementation and felt the need for a task-centric worklist.
To address these drawbacks, we explored other workflow organization techniques implemented in Epic modules in other areas of the hospital, namely the inpatient/emergency department “status boards.” Status boards, commonly found in nursing areas, display key information regarding patient care in an organized way, tailored to that specific area. With this template in mind, we generated a task-centric “status board” within Beaker for use in the histology laboratory. We implemented the status board using Beaker's MyReports module by leveraging tailored report settings (Figure 1B). This status board displayed pending histology lab tasks, priorities, and time-in-status among other task-specific notes that the ordering user may provide. This allowed for triage of urgent cases and helped communicate case-specific needs at-a-glance. The status board has a filter and sort features. This bolsters the user experience, visualizing all specimens that require the same task. For example, the user can filter the status board by “H&E biopsy” tasks and then sort by date received to ensure the oldest tasks are addressed first. While doing this, the user would also be able to note tasks flagged as “RUSH,” as well as specific notes from the grossing staff such as “tiny biopsy, three total pieces.” Lastly, the status board could adapt to changes in slide routing, such as a case being assigned to a different pathologist while in process, which was not possible under the case-prep worklist. When slide tasks are shipped out of the lab, they are automatically removed from the status board, mimicking the actual workflow. Our status board in many ways supplanted the default case-prep worklist used by Beaker.
Our status board is also useful for intraoperative slide logistics. At our institution, all intraoperative slides accompany the tissue cassettes to histology, after specimen grossing. Ideally, all diagnostic case materials would then remain together through histology lab generation of permanent tissue sections from the cassettes. Unfortunately, intraoperative slides would be missed when staff were packing permanent sections for a given case and were not sent to the main hospital. We found that this occurred because there was no indicator to alert the staff to locate intraoperative slides at the time of case packing. An additional benefit of the status board is that it also acts as an inventory for all case materials which need to be shipped to the pathologist at a specific time. Thus, unlike any default Beaker module, we created a status board to display the intraoperative slides to be shipped along with the permanent sections.
Slide volume, compensation, and resident training
Gross tissue specimens are examined by both trained professionals (pathology assistants) as well as pathologists in training (pathology residents). Certain trainee mistakes may be overlooked by mentors and staff. Routine lab volume reporting failed to identify an increase in block volumes from cases prepared by grossing-room trainees. Specifically, excess blocks were submitted for routine mammoplasty (non-cancerous) specimens by trainees. This spike in volume delayed the processing of these specimens and impeded other lab tasks on the days in which excess blocks were submitted. To evaluate the scope and severity of the problem, we developed a data dashboard. This helped to identify the trainees driving the issue. Additionally, these data were used in conjunction with compensation data to visualize the drop in case compensation with the submission of excess blocks (and by extension, slides) on these types of cases (Figure 2A). This visualization proved useful in trainee education and corrected the blocks-per-case levels.
|
Subspecialty-specific turnaround time investigation
Turnaround time (TAT) is calculated from the time of specimen accessioning to the time when the final pathology report is finalized. In 2019, histology leadership was notified by Genitourinary sub-specialist pathologists that our prostate biopsy TAT was slow. This was initially misattributed to a decrease in staffing, which affected the overall histology lab TAT for September to November 2019 (see Figure 2B). The prostate subspecialty-specific drop-in TAT compliance was investigated by building a dynamic TAT reporting dashboard with the capability to filter across multiple variables (e.g., surgical specialty, specimen source, contributing clinic). Using this dashboard, we filtered the cases by prostate subspecialty and client, which revealed that the delay was not due to decreased staffing but rather an idiosyncrasy in case handling. The delayed prostate specimens exclusively belonged to a specific outpatient surgical center. The case handling error was traced to the placement of the biopsies in question in a nonstandard, overlooked location. Correction of the error led to 100 percent TAT compliance by the following month (October 2019, as shown in Figure 2B).
References
- ↑ "What is Data Visualization?". Klipfolio. https://www.klipfolio.com/resources/articles/what-is-data-visualization. Retrieved 19 November 2020.
- ↑ Few, S. (18 September 2004). "Eenie, Meenie, Minie, Moe: Selecting the Right Graph for Your Message" (PDF). Perceptual Edge. http://www.perceptualedge.com/articles/ie/the_right_graph.pdf. Retrieved 19 November 2020.
- ↑ 3.0 3.1 Halwani, F.; Li, W.C.; Banerjee, D. et al. (2016). "A real-time dashboard for managing pathology processes". Journal of Pathology Informatics 7: 24. doi:10.4103/2153-3539.181768. PMC PMC4872478. PMID 27217974. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4872478.
- ↑ Blau, J.L.; Wilford, J.D.; Dane, S.K. et al. (2017). "Implementation of Epic Beaker Anatomic Pathology at an Academic Medical Center". Journal of Pathology Informatics 8: 47. doi:10.4103/jpi.jpi_31_17. PMC PMC5760958. PMID 29387505. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5760958.
- ↑ Albert, C. (2019). "Ups and downs of bringing in Beaker AP LIS". CAP Today (August 2019). https://www.captodayonline.com/ups-and-downs-of-bringing-in-beaker-ap-lis/.
Notes
This presentation is faithful to the original, with only a few minor changes to presentation and updates to spelling and grammar. In some cases important information was missing from the references, and that information was added.